Endometriosis diet is gaining recognition as an important tool in managing the symptoms of this chronic condition. Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, leading to pain, inflammation, and fertility challenges. While medical treatments remain central, research shows that dietary choices can play a powerful role in reducing flare-ups, improving energy levels, and even supporting reproductive health.
The foods you eat can either calm inflammation or worsen it, making nutrition a key factor in daily symptom control. An anti-inflammatory, nutrient-rich eating pattern can help ease pelvic pain, manage bloating, and regulate hormonal balance. At the same time, avoiding certain foods that trigger inflammation may significantly reduce discomfort.
This guide explores evidence-based nutrition strategies for women living with endometriosis. You’ll learn about the best foods for endometriosis pain relief, foods to avoid, natural remedies, supplements, and practical meal planning tips. We’ll also look at how lifestyle choices such as yoga and diet work together for long-term symptom management.
At Mayflower Women’s Hospital, we combine medical expertise with personalized nutrition counseling to create tailored endometriosis diet plans that support both pain relief and fertility goals.
Understanding Endometriosis and the Role of Nutrition
How Endometriosis Affects Hormones and Inflammation
Endometriosis is closely linked to estrogen dominance and chronic inflammation. The misplaced tissue behaves like endometrial lining, thickening and bleeding with each menstrual cycle, but without an outlet. This causes scarring, pelvic pain, and in some cases, fertility issues. The immune system responds with an inflammatory cascade, releasing chemicals that worsen swelling and pain.
Here, diet plays a central role. Certain foods increase estrogen activity or fuel inflammation, while others provide nutrients that regulate hormones and calm inflammatory pathways.
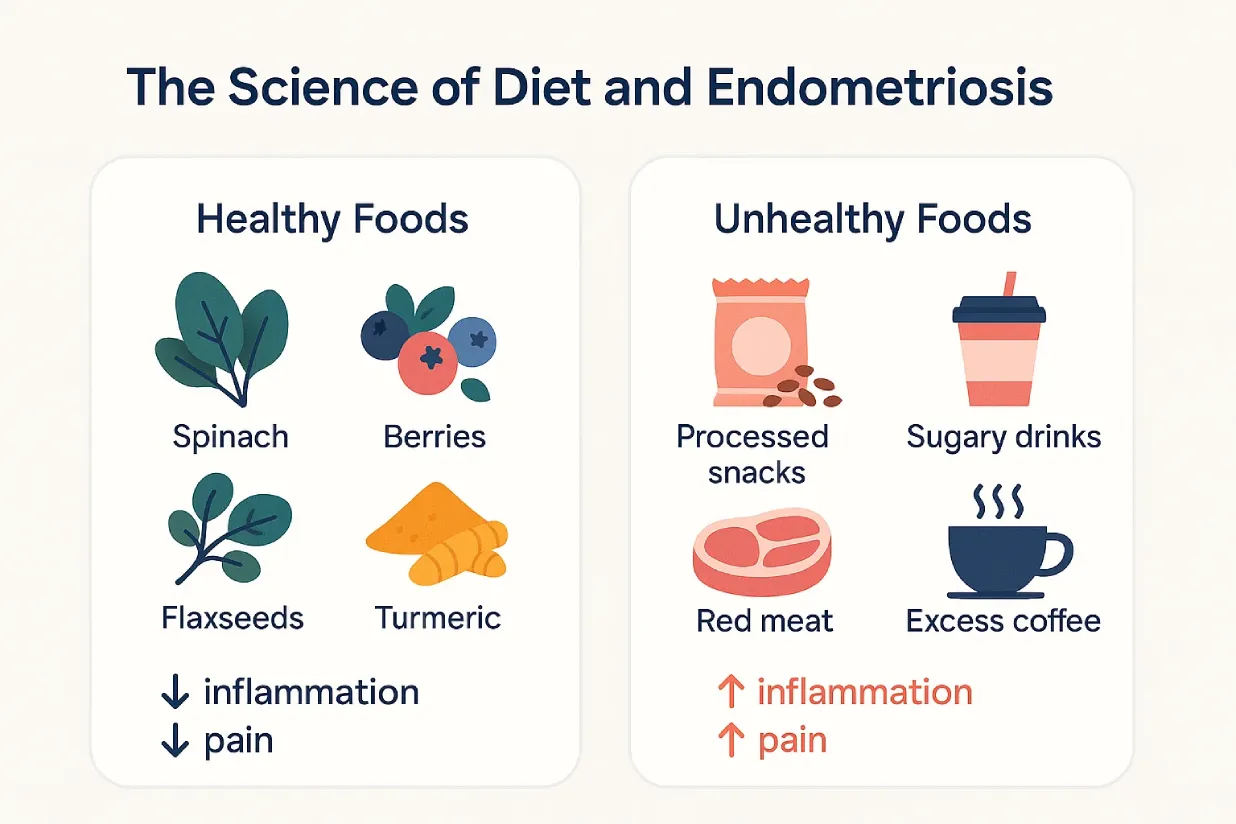
The Science Behind Food and Symptom Management
Food is more than calories-it acts as information for the body. Anti-inflammatory foods such as leafy greens, omega-3 fatty acids, and colorful fruits reduce oxidative stress and help regulate immune response. On the other hand, high-fat processed foods or refined sugars may aggravate endometriosis pain by promoting inflammation.
Nutrients like antioxidants, fiber, and phytoestrogens have shown promising effects in balancing hormone metabolism and improving digestion, both of which are essential for women living with endometriosis.
Evidence from Research on Diet and Endometriosis
- Studies on Anti-inflammatory Diets: Research suggests women following Mediterranean-style or anti-inflammatory diets report fewer pain episodes and better quality of life.
- Impact on Fertility: Diets high in whole grains, fruits, and omega-3s have been linked with improved fertility outcomes in endometriosis patients.
- Gut Health Connection: A fiber-rich diet supports gut microbiota, which influences estrogen metabolism and overall hormonal health.
Understanding the science behind diet and endometriosis is the first step. Next, we’ll look at the best diet for endometriosis, including specific foods that relieve pain, boost fertility, and support long-term well-being.
Best Diet for Endometriosis
Anti-inflammatory Diet for Endometriosis
One of the most effective approaches is an anti-inflammatory diet, which emphasizes whole, nutrient-rich foods that reduce oxidative stress and inflammation. This pattern is similar to the Mediterranean diet, focusing on fresh vegetables, fruits, legumes, lean proteins, nuts, and seeds.
Key benefits of this diet include:
- Reducing pelvic pain and bloating.
- Supporting healthy estrogen metabolism.
- Providing antioxidants that protect against cellular damage.
By choosing anti-inflammatory meals consistently, many women notice gradual but meaningful improvements in daily symptoms.
Foods That Reduce Pain and Inflammation
Specific endometriosis pain relief foods have anti-inflammatory or hormone-regulating properties:
- Leafy greens (spinach, kale, broccoli): packed with antioxidants.
- Berries (blueberries, raspberries): rich in polyphenols that combat oxidative stress.
- Fatty fish (salmon, mackerel, sardines): omega-3 fatty acids that calm inflammation.
- Nuts and seeds (walnuts, flaxseed, chia): plant-based omega-3 sources.
- Turmeric and ginger: natural anti-inflammatory spices used in cooking or teas.
Nutrition for Endometriosis and Fertility
Endometriosis is one of the leading causes of infertility. However, nutrition can support reproductive health by regulating hormones and improving egg quality.
Fertility-friendly diet tips:
- Whole grains (quinoa, oats, brown rice) for steady blood sugar and hormone balance.
- Antioxidant-rich foods (citrus, pomegranate, dark chocolate) to protect eggs from oxidative stress.
- Iron-rich plant foods (lentils, beans, pumpkin seeds) to replenish stores lost due to heavy bleeding.
- Omega-3 sources to improve egg quality and reduce inflammation in the pelvic cavity.

Endometriosis Pain Relief Foods in Daily Life
Adding specific foods into your daily meals can make symptom management easier:
- Start your morning with oatmeal topped with berries and flaxseeds.
- Include grilled salmon or tofu with leafy greens for lunch.
- Use turmeric and ginger in curries, soups, or teas for natural anti-inflammatory support.
These small but consistent changes can significantly ease pain and improve energy levels.
Meal Timing and Portion Control for Better Symptom Management
Endometriosis flare-ups are often linked with digestive distress such as bloating or constipation. Eating smaller, more frequent meals instead of heavy portions can help. Pairing fiber-rich foods with lean proteins also improves digestion and keeps hormones stable.
Practical strategy:
- Three balanced meals + two light snacks per day.
- Stay hydrated with water and herbal teas.
- Avoid skipping meals, as this can worsen fatigue and mood swings.
Now that we’ve explored what to include in an endometriosis-friendly diet, it’s equally important to know what to avoid. The next section outlines common dietary triggers that may worsen inflammation and pain.
Endometriosis Foods to Avoid
Processed and High-fat Foods
Highly processed foods such as packaged snacks, fried items, and fast food are loaded with unhealthy fats, additives, and preservatives. These trigger inflammatory responses in the body, worsening pelvic pain and bloating. Trans fats and saturated fats also interfere with hormone regulation, making endometriosis symptoms more intense.
Tip: Replace fried foods with baked or grilled alternatives, and swap processed snacks for fresh fruits or nuts.
Red Meat and Dairy Concerns
- Red meat has been linked with higher levels of prostaglandins, compounds that can increase uterine contractions and pain. Regular intake of beef, pork, or lamb may also raise estrogen levels, aggravating endometriosis.
- Dairy products like whole milk and full-fat cheese may promote inflammation in some women, particularly if they are sensitive to lactose or casein proteins.
Tip: Consider limiting red meat to occasional meals and replacing with lean poultry or plant proteins. Opt for lactose-free or plant-based dairy alternatives such as almond or oat milk.
Refined Sugar and Caffeine Triggers
Sugary drinks, candies, and desserts cause rapid spikes in blood sugar, leading to increased inflammation and hormonal imbalance. Similarly, excessive caffeine from coffee or energy drinks can elevate stress hormones and worsen anxiety or fatigue in women with endometriosis.
Tip: Choose natural sweeteners like dates or honey in moderation, and switch to herbal teas or green tea instead of multiple cups of coffee.
Why Gluten and Soy Are Sometimes Controversial
Some women with endometriosis report reduced symptoms after eliminating gluten or soy from their diets. Gluten may worsen gut inflammation, while soy contains phytoestrogens that can mimic estrogen in the body. However, research is mixed, and complete elimination is not necessary for everyone.
Tip: Try an elimination diet under medical supervision to identify if gluten or soy triggers your symptoms.
Knowing what to avoid is only half the journey. Many women also benefit from natural remedies and supplements that complement their diet. In the next section, we’ll explore how nutrients, lifestyle habits, and practices like yoga can support endometriosis management.
Natural Remedies and Lifestyle Support
Natural Remedies Endometriosis Diet
Food itself can be a natural remedy. Incorporating plant-based, antioxidant-rich ingredients helps balance hormones and reduce oxidative stress. Herbs and spices like turmeric, ginger, and cinnamon act as natural anti-inflammatories, easing pain without harsh side effects. Fermented foods such as yogurt, kimchi, and kefir support gut health, which plays an important role in estrogen metabolism.
Adopting these dietary remedies gradually builds resilience against flare-ups while improving overall well-being.
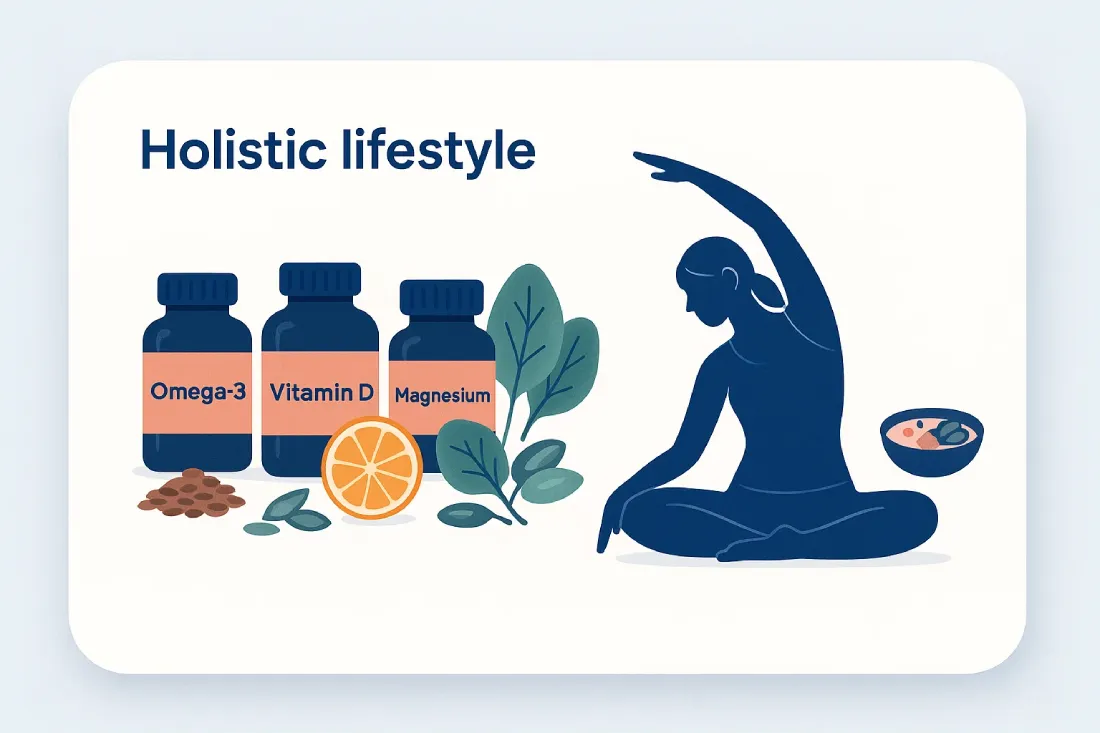
Role of Endometriosis Supplements
Supplements can fill nutritional gaps and complement a healthy diet. Some of the most effective options include:
- Omega-3 fatty acids: Reduce inflammation and menstrual pain.
- Vitamin D: Supports immune regulation and bone health, often deficient in women with endometriosis.
- Magnesium: Relieves muscle tension and reduces cramping.
- Zinc: Helps balance hormone activity and boosts fertility.
Note: Supplements should be taken under medical supervision, as dosage and interactions vary by individual needs.
Omega-3, Vitamin D, Magnesium, Zinc Explained
- Omega-3s from fish oil or flaxseed oil help block prostaglandins that trigger pain.
- Vitamin D deficiency is common in women with endometriosis, and replenishing levels can improve mood and energy.
- Magnesium calms the nervous system, aiding in stress management alongside pain relief.
- Zinc plays a role in egg health and may support women trying to conceive.
Yoga and Diet Endometriosis (Mind-Body Connection)
Lifestyle practices like yoga complement a healthy diet by addressing stress and muscle tension. Yoga postures encourage pelvic relaxation, improve blood circulation, and reduce anxiety. Combined with an anti-inflammatory diet, yoga builds a holistic system for managing both physical and emotional symptoms of endometriosis.
For instance:
- Gentle yoga stretches before bedtime can improve sleep quality.
- Breathing exercises (pranayama) lower stress hormones that may otherwise worsen pain.
- Pairing yoga practice with a light, anti-inflammatory dinner supports better digestion and hormone regulation.
Diet and lifestyle remedies provide a strong foundation, but putting them into practice daily can be overwhelming. The next section offers a practical framework-sample meal plans, grocery lists, and simple tips-to make endometriosis nutrition sustainable.
Practical Framework for Daily Nutrition
Sample One-day Endometriosis Diet Plan
A vegetarian diet rich in anti-inflammatory foods can effectively support women with endometriosis in India. Here’s a sample plan designed to reduce pain, balance hormones, and maintain energy:
- Breakfast: Vegetable upma with turmeric and curry leaves, paired with green tea.
- Snack: A bowl of papaya with soaked walnuts and flaxseeds.
- Lunch: Quinoa khichdi with spinach, carrots, and beans, served with a side of cucumber raita made from plant-based yogurt.
- Snack: Roasted chickpeas or sprouted moong salad with lemon and ginger.
- Dinner: Masoor dal soup with brown rice and sautéed broccoli, finished with turmeric milk (plant-based option like almond or oat milk).
This vegetarian pattern emphasizes whole grains, legumes, nuts, seeds, and antioxidant-rich vegetables.
Breakfast, Lunch, Dinner, Snacks
- Breakfast focus: High-fiber Indian staples like upma, poha, or oats enriched with seeds and nuts.
- Lunch focus: Dal-based proteins (lentils, beans) paired with greens and whole grains like quinoa or brown rice.
- Snack focus: Sprouts, roasted pulses, or fruits with anti-inflammatory spices (ginger, turmeric).
- Dinner focus: Light lentil soups, steamed vegetables, or salads to improve digestion and reduce night-time bloating.
Grocery List for Endometriosis-friendly Meals
A vegetarian-friendly grocery list tailored for Indian kitchens includes:
- Proteins: Lentils (masoor, moong, toor), chickpeas, kidney beans, sprouts, tofu.
- Vegetables: Spinach, kale, broccoli, bottle gourd, carrots, sweet potatoes.
- Fruits: Papaya, pomegranate, citrus fruits, blueberries (if available).
- Whole Grains: Quinoa, brown rice, oats, millet varieties (jowar, bajra, ragi).
- Healthy Fats: Mustard oil, olive oil, chia seeds, flaxseeds, walnuts.
- Spices & Herbs: Turmeric, ginger, garlic, cumin, cinnamon.
- Supplements (if advised): Omega-3 (from flaxseed oil), Vitamin D, Magnesium.
Meal Prep & Budget-friendly Tips
Vegetarian diets can be economical and highly nutrient-dense with a little planning:
- Batch cooks dals and whole grains like millet or quinoa on weekends.
- Soak and sprout beans in advance for easy snacks or salads.
- Use seasonal local vegetables for affordability and freshness.
- Spice-based remedies (like turmeric-ginger teas) double as natural pain relief.
These practical steps make following the best diet for endometriosis easier and sustainable for everyday Indian households.
With a vegetarian framework in place, the next step is to explore different dietary approaches-from Mediterranean to gluten-free-to see how they compare with endometriosis-specific diets.
Comparing Diet Approaches
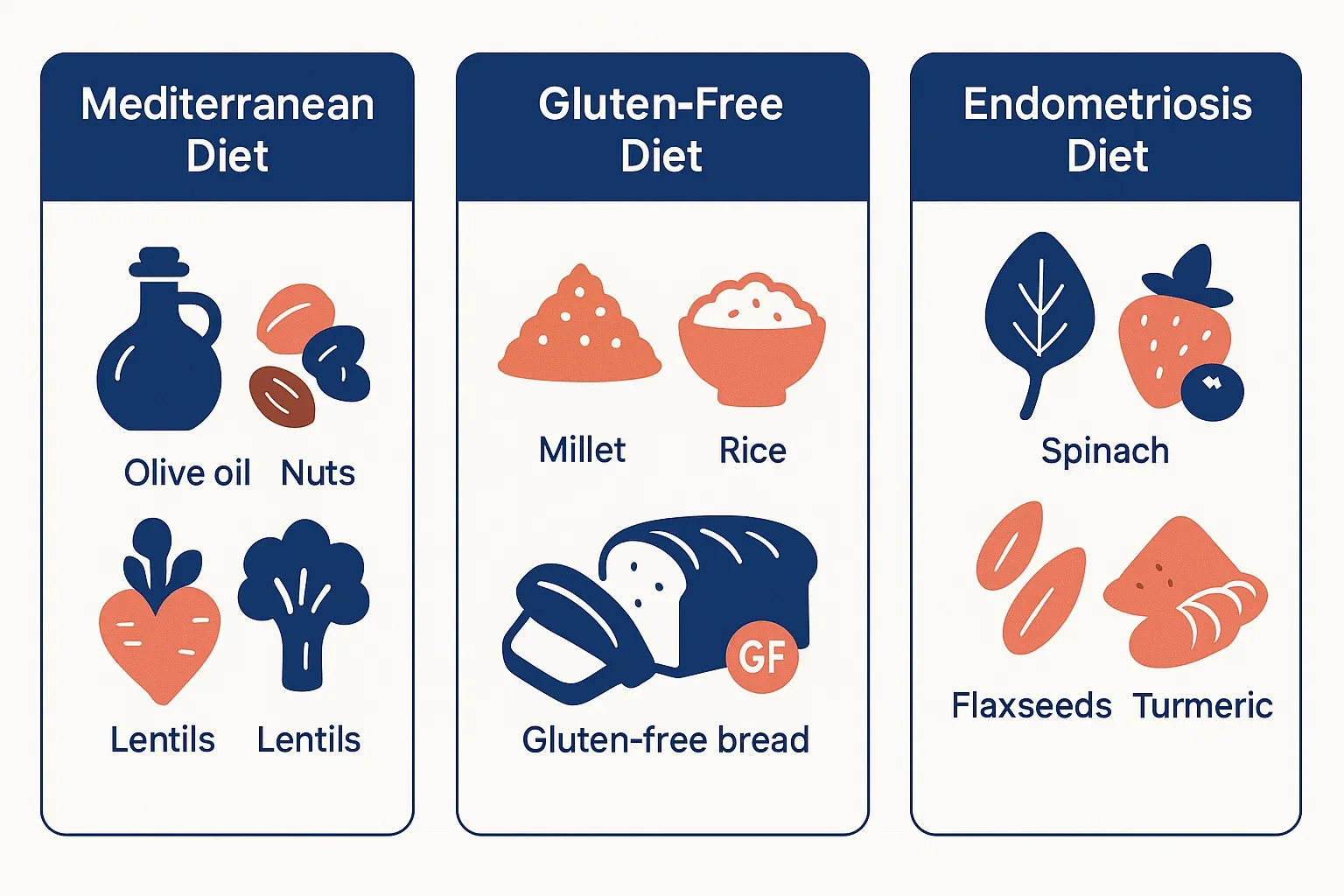
Endometriosis Diet vs General Anti-inflammatory Diet
The endometriosis diet is designed with a sharper focus on hormonal balance and pain management, whereas a general anti-inflammatory diet aims to reduce inflammation overall. Both emphasize vegetables, fruits, nuts, seeds, and whole grains. However, the endometriosis-specific approach also limits foods that may raise estrogen levels or trigger pain-such as red meat, refined sugar, and processed foods.
Takeaway: Women with endometriosis benefit from a more tailored approach that goes beyond standard anti-inflammatory guidelines.
Mediterranean Diet vs Gluten-free Diet for Endometriosis
- Mediterranean Diet: Rich in olive oil, legumes, whole grains, fresh vegetables, and nuts, this diet is strongly backed by research for reducing inflammation and supporting fertility. It aligns closely with the best diet for endometriosis and can be easily adapted to vegetarian Indian preferences using pulses, lentils, and millets.
- Gluten-free Diet: Some women with endometriosis report fewer flare-ups after cutting gluten, especially if they experience bloating or digestive issues. However, research is limited, and not all women need to avoid gluten. Eliminating wheat, barley, and rye should be tried cautiously and preferably under medical guidance.
Takeaway: The Mediterranean diet is more universally beneficial, while gluten-free can help those with specific sensitivities.
When to Seek a Personalized Diet Plan
While general diet frameworks are helpful, many women require individualized nutrition guidance to match their symptoms, lifestyle, and fertility goals. For example:
- A woman experiencing severe pain may need higher anti-inflammatory food intake and supplements.
- Someone preparing for fertility treatment might focus on antioxidants, folate, and iron.
- Women with digestive discomfort may benefit from gluten or dairy elimination trials.
This is where a Mayflower endometriosis diet plan becomes valuable. A customized program combines medical insights with nutritional strategies to create sustainable, long-term results.
Now that we’ve compared different diets, the next step is to look at how Mayflower integrates medical care with nutrition counseling, providing patients with a holistic, personalized path to endometriosis management.
Mayflower’s Endometriosis Diet Plan & Counseling
Personalized Nutrition Plans at Mayflower
Every woman with endometriosis experiences symptoms differently. While some struggle with pain, others face fertility challenges, fatigue, or digestive distress. At Mayflower Women’s Hospital, our specialists design personalized endometriosis diet plans tailored to your body’s unique needs. These plans combine balanced nutrition, supplements (where required), and lifestyle modifications to support long-term relief.
Unlike generic online diets, Mayflower’s programs are developed in collaboration with gynecologists and dietitians who understand the complex hormonal changes linked with endometriosis.
Medical and Dietary Support Combined
Managing endometriosis often requires more than medication alone. At Mayflower, we integrate dietary guidance with medical care to address the condition from multiple angles:
- Nutrition counseling: Practical advice on meal choices, grocery planning, and portion control.
- Medical monitoring: Tracking pain levels, cycle regularity, and fertility outcomes alongside dietary changes.
- Supplement guidance: Safe use of omega-3, vitamin D, or magnesium when clinically beneficial.
- Lifestyle integration: Combining yoga, stress management, and sleep hygiene with dietary support.
This holistic model empowers women to take control of their condition while benefiting from evidence-based care.
Endometriosis Support Groups and Counseling at Mayflower
Dietary changes are easier to sustain with community and professional support. Mayflower offers endometriosis support groups and one-on-one counseling sessions where women can share their journeys, learn coping strategies, and stay motivated. Emotional well-being is treated as an essential part of recovery, alongside medical and dietary care.
These programs provide:
- Guidance on food planning during flare-ups.
- Encouragement from peers who understand your challenges.
- Access to expert counseling for stress and anxiety related to endometriosis.
With personalized diet plans, integrated medical care, and emotional support, Mayflower ensures women receive complete guidance for managing endometriosis. In the next section, we’ll provide practical coping tips you can start applying today for consistent pain relief and better quality of life.
Practical Tips for Coping with Endometriosis Through Food
Easy Meal Prep for Symptom Relief
Meal preparation is one of the simplest ways to stay consistent with the endometriosis diet. Preparing ingredients ahead of time reduces stress on days when pain is intense and makes it easier to avoid unhealthy choices.
- Cook dals, legumes, and grains in bulk and store them for quick use.
- Keep roasted seeds and nuts handy for nutrient-rich snacks.
- Prepare spice blends with turmeric, cumin, and ginger to easily add anti-inflammatory benefits to meals.
Building a Long-term Sustainable Diet
Many women find it difficult to follow strict diets for extended periods. The goal is not perfection, but consistency. Focus on adding more anti-inflammatory foods rather than obsessing about restrictions.
- Replace fried snacks with roasted or steamed options.
- Add at least one green vegetable to every meal.
- Drink plenty of water and herbal teas throughout the day.
- Enjoy seasonal Indian fruits like papaya, guava, and pomegranate, which are naturally supportive for hormone balance.
Small Daily Habits That Make a Difference
Lifestyle and food choices, when combined, offer better results:
- Practice mindful eating: Chew slowly to improve digestion and reduce bloating.
- Pair diet with movement: Gentle yoga or walking after meals can reduce cramps and stress.
- Track your diet and symptoms: Keeping a food diary helps identify which foods trigger or relieve pain.
- Stay flexible: If dining out, choose simple dishes like lentil soups, salads, or steamed vegetables.
By making small but consistent dietary adjustments, women with endometriosis can gradually regain control over their symptoms and quality of life. The next section will summarize the key lessons and highlight how professional guidance at Mayflower can make this journey smoother and more effective.
Conclusion
Diet alone cannot cure endometriosis, but it can make a meaningful difference in how women experience daily life with the condition. Choosing an endometriosis diet focused on anti-inflammatory foods, whole grains, legumes, fruits, and seeds helps reduce pain, balance hormones, and support fertility. At the same time, avoiding processed foods, excess sugar, and red meat can prevent flare-ups and digestive discomfort.
Nutrition is most effective when combined with other supportive practices like supplements, yoga, and stress management. Together, these elements form a holistic strategy that addresses both physical and emotional challenges.
However, every woman’s journey with endometriosis is unique. Some may benefit from eliminating gluten, while others may see improvements simply by adding more fiber and antioxidants. This is why personalized dietary guidance makes a significant difference.
At Mayflower Women’s Hospital, we integrate advanced medical treatment with individualized endometriosis diet plans, helping women manage pain, improve fertility, and regain confidence in their daily lives. With expert gynecologists, experienced dietitians, and supportive counseling, we provide a complete care pathway for women navigating this condition.
If you’re ready to take control of your symptoms, start by making small dietary changes today-and consider consulting with our specialists at Mayflower for a plan tailored to your body and lifestyle.
FAQ
Foods rich in anti-inflammatory compounds such as leafy greens, berries, flaxseeds, walnuts, and turmeric can reduce swelling and discomfort. Including these daily may ease pelvic pain and improve energy levels.
Yes. A diet high in whole grains, antioxidants, and omega-3 fatty acids supports hormonal balance, egg quality, and uterine health. These nutrients create a healthier environment for conception.
It is best to limit processed snacks, red meat, sugary desserts, and excess caffeine, as these may trigger inflammation and hormonal imbalance. Some women also benefit from reducing dairy or gluten.
Supplements such as omega-3 fatty acids, vitamin D, magnesium, and zinc can help reduce inflammation, regulate hormones, and improve fertility. Always consult a doctor before starting any supplement routine.
At Mayflower Women’s Hospital, nutritionists and gynecologists work together to design diet plans tailored to your symptoms, fertility goals, and lifestyle. These plans combine meal guidance, supplement advice, and ongoing counseling for sustainable results.
Author
-

Dr. Smeet, true to his name, is known for his warm personality and cheerful smile that make patients instantly feel at ease with him.
Until now, he has performed 8000+ surgeries and several of which are supra-major surgeries for deep infiltrating endometriosis and fertility enhancing surgeries. With several publications in notable journals, he is constantly pushing the envelope of possibilities in gynecological surgeries