Fibroids are one of the most common gynecological conditions affecting women in their reproductive years, yet they often remain undiagnosed until symptoms become difficult to ignore. These noncancerous growths, also called uterine fibroids, develop within or around the uterus and can vary widely in size from tiny nodules to large masses that alter the shape of the uterus.
While some women may never experience discomfort, others struggle with fibroid symptoms such as heavy bleeding, pelvic pressure, and chronic pain. For many, questions like “Do fibroids cause pain all the time?” or “Can fibroids affect pregnancy?” become urgent concerns. Because every woman’s experience is unique, understanding the underlying fibroids causes, risk factors, and early warning signs is crucial.
Over the years, advancements in medical science have transformed the way fibroid diagnosis and treatment are managed. From imaging tools like ultrasound and MRI to minimally invasive surgeries and advanced robotic-assisted procedures, today’s options are safer, faster, and more personalized. Women can now choose from a range of approaches non-surgical, medical, or surgical depending on their health goals, fertility needs, and symptom severity.
This comprehensive guide explains the symptoms, diagnosis, and latest treatments for fibroids, while also addressing their impact on fertility and pregnancy. By the end, you will gain clear insights into when to seek care, what treatment choices exist, and how modern gynecology is improving outcomes for women living with fibroids.
Understanding Fibroids in Women’s Health
What Are Uterine Fibroids?
Uterine fibroids are noncancerous growths made of muscle and connective tissue that develop within the uterus. They are medically known as leiomyomas or myomas. Though benign, they can cause significant discomfort depending on their size, number, and location.
Fibroids are among the most common conditions in women’s health, affecting up to 70–80% of women by the age of 50. Some women may not realize they have them until they undergo a routine pelvic exam or imaging test.
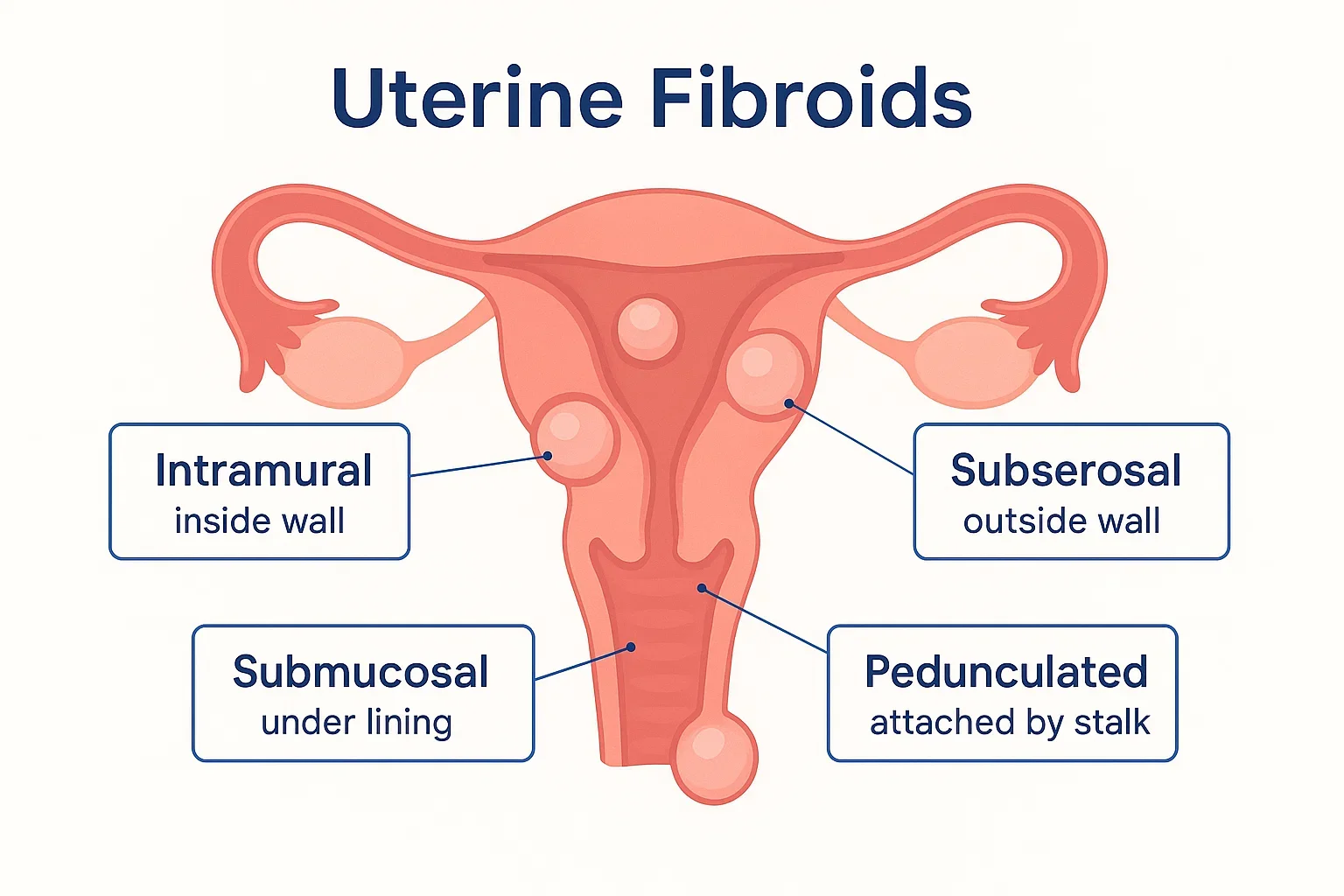
Types of Fibroids
Fibroids are classified based on where they grow in the uterus:
- Intramural fibroids – grow within the muscular wall of the uterus and are the most common.
- Subserosal fibroids – develop on the outer wall of the uterus, sometimes pressing on nearby organs.
- Submucosal fibroids – form just beneath the uterine lining, often linked with heavy menstrual bleeding and fertility problems.
- Pedunculated fibroids – attached to the uterus by a thin stalk and may twist, causing sudden pain.
Understanding the type of fibroid helps doctors determine the best fibroid treatment plan.
Fibroids vs Cysts – What’s the Difference?
It is common for women to confuse fibroids vs cysts, as both can cause abdominal pain or pelvic pressure. The difference lies in their structure:
- Fibroids are solid muscle tumors that form in or on the uterus.
- Cysts are fluid-filled sacs, typically found on the ovaries.
Unlike fibroids, cysts often disappear on their own, whereas fibroids usually persist or grow over time and may require treatment.
Fibroids Symptoms Every Woman Should Watch
Fibroids do not always cause problems, but when they do, the symptoms can affect a woman’s daily life, energy levels, and reproductive health. Recognizing early fibroids symptoms helps in timely diagnosis and treatment.
Menstrual-Related Symptoms
One of the most common signs of fibroids is abnormal menstrual bleeding. Women may experience:
- Heavy periods that soak through pads or tampons in less than two hours.
- Prolonged periods lasting more than seven days.
- Passage of large blood clots during menstruation.
These changes may lead to anemia, causing fatigue, dizziness, and weakness.
Pain-Related Symptoms
Many women wonder, “Do fibroids cause pain all the time?” The answer is no pain depends on the size and location of the fibroid. However, fibroids often cause:
- Pelvic pain or pressure, sometimes radiating to the lower back or thighs.
- Cramps outside of the normal menstrual cycle.
- Pain during intercourse, depending on fibroid placement.
This fibroid pain may be dull and persistent or sharp and sudden, especially if a fibroid outgrows its blood supply.
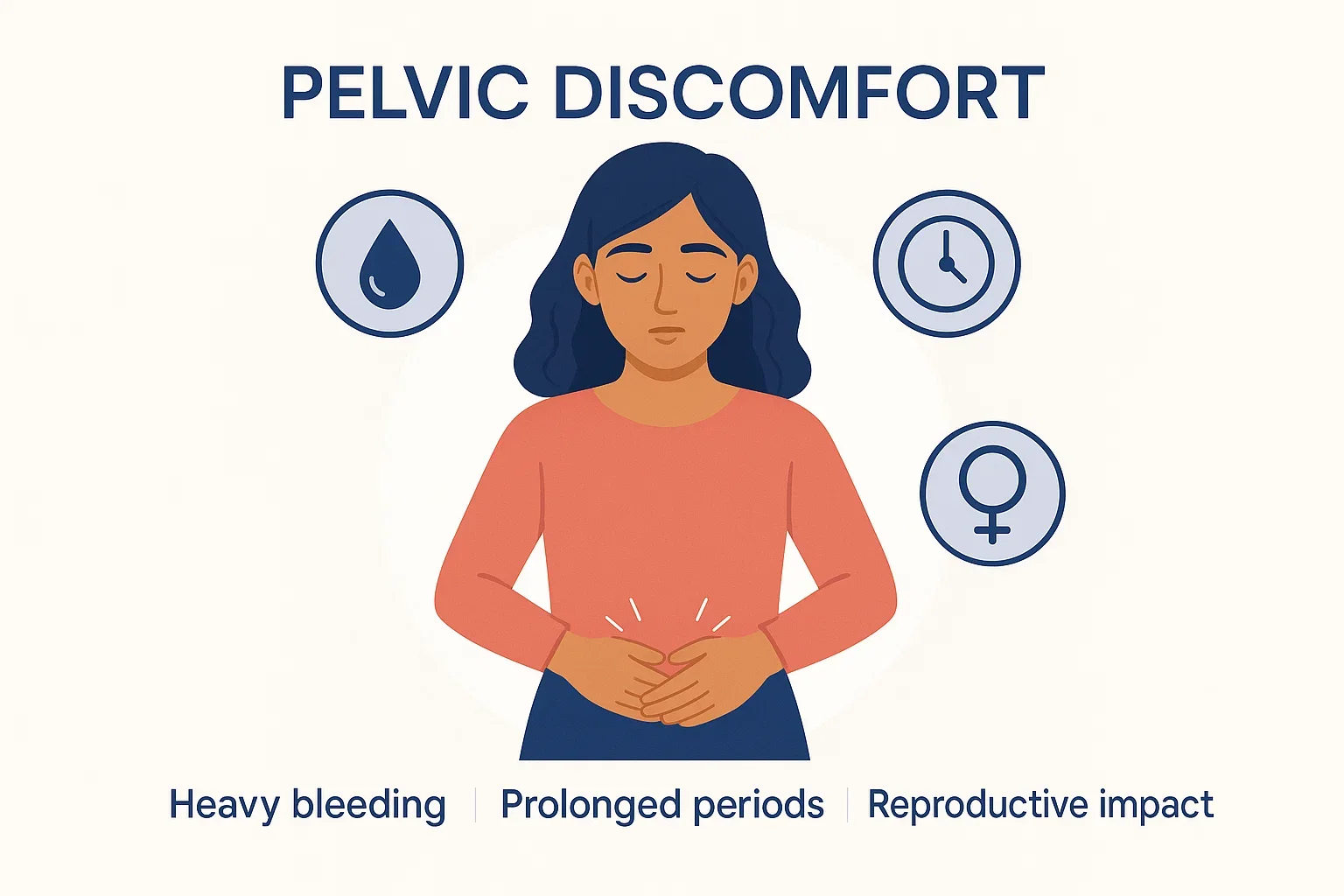
Reproductive and Bladder-Related Symptoms
Fibroids can also interfere with fertility and affect nearby organs:
- Difficulty conceiving or recurrent miscarriages.
- Complications during pregnancy, such as preterm labor.
- Frequent urination when fibroids press against the bladder.
- Constipation or bloating if they press on the rectum.
When to See a Doctor
Not every case of fibroids requires immediate treatment, but you should seek medical care if you notice:
- Periods that disrupt your routine or require double protection.
- Persistent pelvic pain or abdominal swelling.
- Difficulty becoming pregnant or carrying a pregnancy to term.
Early consultation ensures that symptoms are managed effectively before complications arise.
Causes and Risk Factors of Fibroids
While the exact fibroids causes are not fully understood, research shows that multiple biological and lifestyle factors influence their development. Knowing these risk factors helps women identify when they may be more vulnerable.
Biological Causes
- Hormonal influence – Fibroids are closely linked to estrogen and progesterone, the hormones that regulate the menstrual cycle. Higher levels can encourage fibroid growth, which is why they often shrink after menopause.
- Genetic predisposition – Women with a family history of uterine fibroids are more likely to develop them. Specific gene mutations have also been linked to fibroid formation.
Lifestyle and Demographic Factors
- Age – Fibroids are most common in women aged 30–45, though they can appear earlier.
- Ethnicity – Studies show women of African descent are more prone to fibroids and may experience them at younger ages with more severe symptoms.
- Obesity – Excess body fat can raise estrogen levels, contributing to fibroid growth.
- Stress and diet – High-stress lifestyles and diets rich in processed foods may increase the risk.
Myths vs Facts
Many misconceptions surround fibroids:
- Myth: All fibroids cause symptoms.
- Fact: Many fibroids are small and harmless, requiring no treatment.
- Myth: Fibroids always need surgery.
- Fact: Non-surgical options and lifestyle changes can manage symptoms effectively.
- Myth: Fibroids turn into cancer.
- Fact: Fibroids are almost always benign; malignant transformation is extremely rare.
How Doctors Diagnose Fibroids
Accurate fibroid diagnosis is essential for planning the right treatment. Since many women confuse fibroid symptoms with other gynecological conditions, doctors rely on a combination of medical history, clinical examination, and imaging techniques.

Clinical Examination
A gynecologist often begins with a pelvic exam to check for:
- Enlarged uterus
- Irregularities in shape
- Firm masses that may indicate uterine fibroids
While a pelvic exam can raise suspicion, imaging tests are usually needed for confirmation.
Imaging Tools for Fibroid Detection
- Ultrasound – This is the first-line tool for detecting fibroids. A transabdominal ultrasound provides a broad view of the uterus, while a transvaginal ultrasound offers clearer detail of smaller fibroids.
- MRI (Magnetic Resonance Imaging) – Offers high-resolution images to map fibroid size, number, and location. MRI is especially useful in planning surgery or advanced treatments.
Invasive Procedures for Complex Cases
In some situations, doctors may need direct visualization of the uterus:
- Hysteroscopy – A thin telescope-like device inserted through the vagina to view the uterine cavity.
- Laparoscopy – A minimally invasive procedure using a camera through a small incision in the abdomen to check the uterus and surrounding organs.
These tests are helpful when fibroids are difficult to detect or when other conditions may mimic fibroid symptoms.
Differential Diagnosis
Because symptoms of fibroids overlap with other conditions, doctors may also rule out:
- Ovarian cysts – fluid-filled sacs that differ from fibroids.
- Endometriosis – tissue growth outside the uterus that can cause pain.
- Adenomyosis – thickening of the uterine wall, often mistaken for fibroids.
A precise diagnosis ensures women receive the most effective and least invasive treatment.
Fibroids During Pregnancy: What Women Need to Know
Pregnancy can be a joyful milestone, but the presence of fibroids during pregnancy may introduce additional challenges. While many women with fibroids carry healthy pregnancies, the size, number, and location of fibroids can influence outcomes.
How Fibroids Affect Pregnancy
Fibroids may grow in response to higher estrogen levels during pregnancy. Depending on their placement, they can:
- Distort the uterine cavity, increasing the risk of miscarriage.
- Cause fibroid pain due to rapid growth or degeneration.
- Lead to complications such as preterm labor, breech position, or placental abruption.
Not all fibroids cause problems, but monitoring is crucial.
Risks for Mother and Baby
Some of the possible risks associated with fibroids in pregnancy include:
- Miscarriage – particularly with submucosal fibroids.
- Restricted fetal growth if fibroids reduce available space in the uterus.
- Labor complications, making vaginal delivery difficult and sometimes requiring a cesarean section.
Managing Fibroids During Pregnancy
Doctors usually take a conservative approach during pregnancy, focusing on:
- Regular ultrasounds to monitor fibroid growth.
- Pain management with safe medications when needed.
- Delivery planning, which may include cesarean section if fibroids obstruct the birth canal.
After delivery, fibroids may shrink naturally as hormone levels return to normal. In some cases, treatment is delayed until after childbirth to ensure the safest outcome for both mother and baby.
Fibroids Treatment Options Explained
Not all fibroids require immediate treatment. Some remain small and cause no symptoms, while others lead to heavy bleeding, pain, or fertility challenges. The right fibroids treatment depends on the severity of symptoms, age, reproductive goals, and overall health.
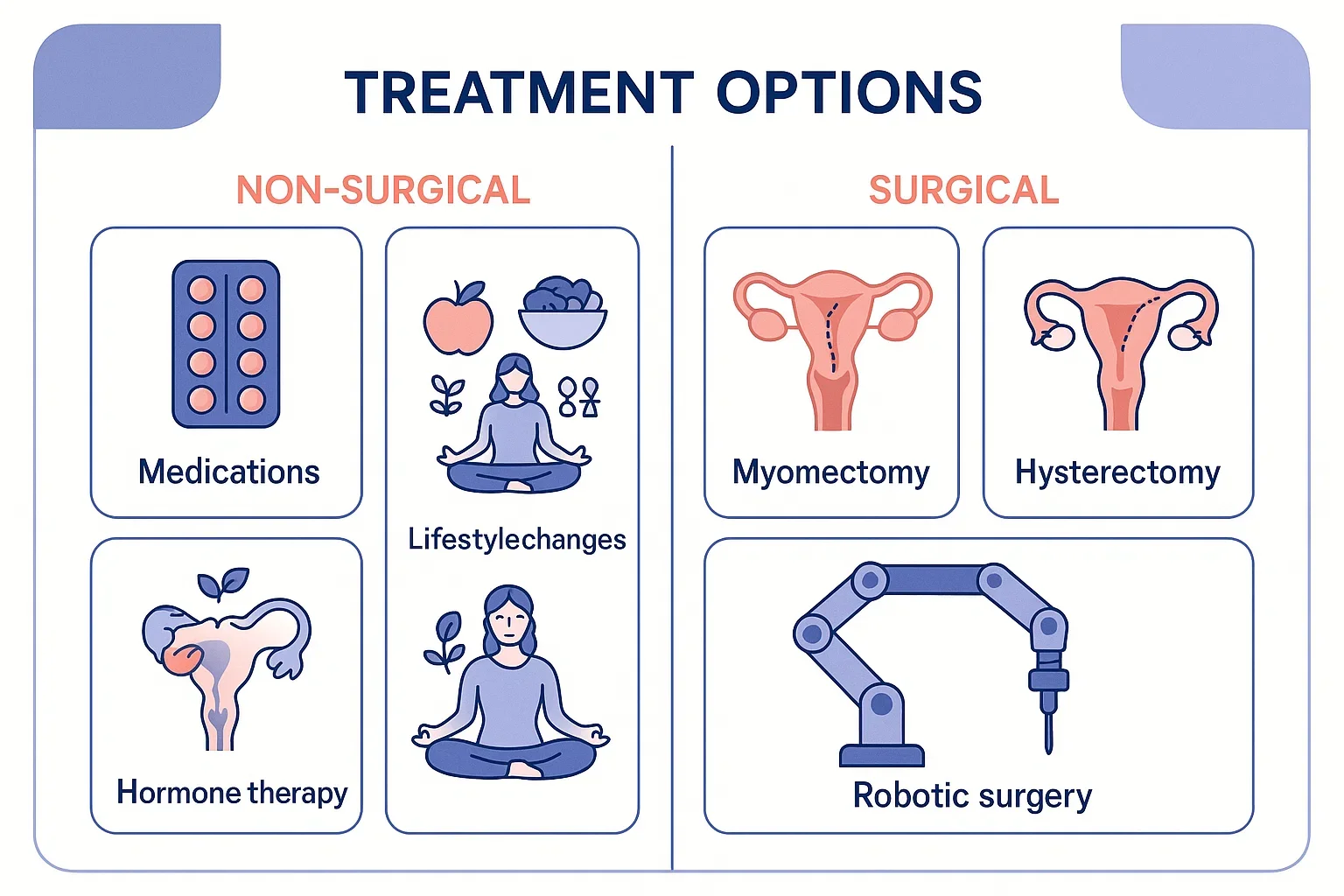
Non-Surgical Treatments
For women with mild symptoms, conservative approaches may be enough.
- Medications – Hormonal treatments, such as birth control pills or progesterone-releasing IUDs, can help control heavy bleeding. Gonadotropin-releasing hormone (GnRH) agonists may temporarily shrink fibroids by lowering estrogen levels.
- Pain relief – Over-the-counter anti-inflammatory medications can reduce fibroid pain anemia due to heavy bleeding and discomfort during periods.
- Lifestyle adjustments – Regular exercise, a balanced diet, and stress management may help reduce symptoms and improve quality of life, although they do not eliminate fibroids.
These methods are best suited for women who do not want surgery and whose fibroids are not severely impacting fertility or daily life.
Minimally Invasive Treatments
Modern medicine offers several minimally invasive procedures that shrink or remove fibroids while preserving the uterus:
- Uterine Artery Embolization (UAE) – A procedure where blood supply to fibroids is blocked, causing them to shrink over time. It is effective for symptom relief but may affect future pregnancy options.
- MRI-Guided Focused Ultrasound Surgery (FUS) – A non-invasive treatment that uses high-frequency ultrasound waves to destroy fibroid tissue. Recovery is quick, but availability is limited.
- Radiofrequency Ablation (RFA) – Uses heat energy to shrink fibroids, usually performed laparoscopically.
These techniques are preferred by women seeking alternatives to open surgery.
Fibroids Surgery
When fibroids are large, symptomatic, or interfering with fertility, surgery may be the best option.
- Myomectomy – A fertility-preserving surgery where fibroids are removed while keeping the uterus intact. It can be performed through hysteroscopy, laparoscopy, or open abdominal surgery. Myomectomy is often recommended for women who wish to conceive in the future.
- Hysterectomy – A definitive surgery where the uterus is removed. It is the only guaranteed cure for fibroids but eliminates the possibility of future pregnancies. Hysterectomy may be recommended if fibroids are recurrent, very large, or severely symptomatic.
Recovery timelines vary depending on the type of surgery. Minimally invasive procedures often require just a few days, while open surgeries may take several weeks.
Choosing the Right Treatment
The decision between medication, minimally invasive therapy, or surgery should always be made with a gynecologist. Factors such as age, family planning, fibroid size, and symptom severity guide the treatment plan.
Latest Advances in Fibroid Care
The field of gynecology has seen remarkable progress in the management of fibroids. Today, women have access to safer, more effective, and less invasive treatments than ever before. These latest fibroid treatments aim to reduce symptoms, shorten recovery times, and preserve fertility whenever possible.
Robotic-Assisted Surgery
Robotic myomectomy and hysterectomy use advanced robotic systems to improve precision. Surgeons operate with enhanced 3D visualization, which allows for smaller incisions, less blood loss, and quicker recovery compared to traditional surgery.
Targeted Hormonal Therapies
Newer medications that selectively block hormones are changing the way doctors manage fibroids. For example, selective progesterone receptor modulators (SPRMs) can shrink fibroids without triggering the extreme side effects seen with older hormone therapies.
Personalized Treatment Approaches
Doctors now use advanced imaging and diagnostic tools to map fibroid size and location. This enables them to tailor treatments whether minimally invasive, surgical, or medical according to the woman’s fertility goals and lifestyle.
Future Directions in Fibroid Management
Research is underway into genetic and molecular therapies that may one day prevent fibroids from forming. Scientists are also exploring regenerative medicine to repair the uterus after fibroid removal, further improving outcomes for women who wish to have children.
With these innovations, fibroid care is moving beyond symptom control to comprehensive solutions that improve long-term reproductive health and overall quality of life.
Living with Fibroids: Coping & Lifestyle Management
Even when treatment is not immediately required, managing the impact of uterine fibroids on daily life is important. Lifestyle choices, regular monitoring, and emotional support can make a significant difference in overall well-being.
Diet and Nutrition
Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins supports hormone balance. Limiting processed foods, caffeine, and red meat may help reduce inflammation and ease fibroid pain. Iron-rich foods are also important for women who experience heavy menstrual bleeding.
Exercise and Stress Management
Regular physical activity improves circulation, reduces stress, and helps maintain healthy weight factors that may slow fibroid growth. Stress management techniques such as yoga, meditation, or breathing exercises can reduce the severity of symptoms.
Routine Medical Checkups
Even if fibroids are small, regular gynecological checkups and ultrasounds are necessary to monitor changes. Early detection of growth or complications allows for timely fibroid treatment when needed.
Emotional and Social Support
Fibroids can affect more than physical health; they may also influence confidence, relationships, and emotional well-being. Support groups, counseling, or open discussions with loved ones can provide much-needed encouragement.

By combining medical guidance with healthy lifestyle habits, women can manage fibroids more effectively and maintain a higher quality of life.
Fibroids and Fertility: What Patients Should Know
Fibroids can influence a woman’s ability to conceive and maintain a healthy pregnancy. While not every case leads to complications, understanding the connection between fibroids and fertility is essential for women planning to have children.
How Fibroids Affect Fertility
The impact of fibroids depends on their size and location:
- Submucosal fibroids can distort the uterine lining, making it harder for an embryo to implant.
- Intramural fibroids may reduce blood flow to the uterus, affecting embryo development.
- Large fibroids can block fallopian tubes, preventing fertilization.
In some women, fibroids may also increase the risk of miscarriage or repeated pregnancy loss.
Role of Fibroid Surgery in Fertility
For women experiencing infertility, a myomectomy surgical removal of fibroids while preserving the uterus can significantly improve the chances of conception. Advances in minimally invasive techniques mean that recovery is quicker, and future pregnancies are safer.
In contrast, hysterectomy eliminates the possibility of pregnancy and is considered only when family planning is complete.
When to Seek Specialist Help
Women who have difficulty conceiving or who experience multiple miscarriages should consult a fertility specialist. A personalized plan that combines fibroid management with fertility care offers the best outcomes.
Choosing the Right Care for Fibroids
When it comes to managing fibroids, choosing the right healthcare provider is just as important as selecting the right treatment. Because symptoms and outcomes vary widely, expert evaluation ensures that women receive care tailored to their unique needs.
Importance of Specialized Gynecologists
A gynecologist with experience in fibroid management can distinguish between different types of fibroids, assess risks, and recommend the most effective options. From fibroid diagnosis to advanced surgical planning, specialized knowledge makes treatment safer and more precise.
Advanced Facilities and Technology
Hospitals equipped with modern diagnostic tools such as high-resolution ultrasound and MRI can detect fibroids with greater accuracy. Access to minimally invasive procedures, robotic-assisted surgeries, and comprehensive post-treatment care further improves patient outcomes.
Patient-Centered Approach
The best care goes beyond medical treatment. It involves listening to patient concerns, explaining every option, and addressing fertility goals or pregnancy plans. This approach ensures women feel supported throughout their journey with fibroids.
Taking the Next Step
If you are experiencing symptoms such as heavy periods, pelvic pain, or difficulty conceiving, consulting a specialist can bring clarity and relief. Early action prevents complications and allows you to explore treatment options that fit your lifestyle.
Don’t ignore the signs of fibroids, schedule a consultation with a trusted gynecology team to discuss the best path forward for your health.
Conclusion
Fibroids are a common women’s health condition that can range from silent and harmless to painful and life-disrupting. Recognizing early fibroid symptoms, understanding the underlying causes, and seeking timely diagnosis are key to preventing complications. With today’s advanced options from non-surgical therapies and minimally invasive procedures to comprehensive fibroids surgery treatment can be tailored to a woman’s health needs, fertility goals, and lifestyle.
Living with fibroids does not mean living with constant discomfort. By combining medical guidance with supportive lifestyle choices, women can manage symptoms effectively and maintain a high quality of life.
If you or a loved one are experiencing symptoms such as heavy bleeding, pelvic pressure, or infertility concerns, don’t delay. Reach out to our trusted gynecology specialist at Mayflower hospital to explore the best solutions for long-term health and well-being.
FAQs on Fibroids
Not always. Some women experience constant fibroid pain, while others only notice discomfort during periods, pregnancy, or when fibroids grow quickly. Pain severity depends on the fibroid’s size and location.
Fibroids are almost always benign. In very rare cases, they may be linked to a type of cancer called leiomyosarcoma, but this occurs in less than 1% of cases. Regular monitoring helps ensure safety.
Fibroids vs cysts is a common confusion. Fibroids are solid muscle growths that develop in or on the uterus, while cysts are fluid-filled sacs usually found on the ovaries. Their treatments and outcomes differ.
Yes. Fibroids may interfere with embryo implantation, increase the risk of miscarriage, or cause pregnancy complications. However, many women with fibroids still conceive naturally and carry healthy pregnancies.
Recovery depends on the procedure. Minimally invasive surgeries like laparoscopic myomectomy may require only a week or two, while open surgery or hysterectomy may take up to six weeks.
Author
-

Dr. Smeet, true to his name, is known for his warm personality and cheerful smile that make patients instantly feel at ease with him.
Until now, he has performed 8000+ surgeries and several of which are supra-major surgeries for deep infiltrating endometriosis and fertility enhancing surgeries. With several publications in notable journals, he is constantly pushing the envelope of possibilities in gynecological surgeries