Postpartum depression is a serious mental health condition that affects many women after childbirth, going far beyond the usual “baby blues.” While it is natural for new mothers to feel overwhelmed, tired, or emotional during the first few weeks, postpartum depression (PPD) is more intense and longer lasting. It can interfere with a mother’s ability to bond with her baby, manage daily life, and maintain her overall well-being.
Raising awareness about postpartum depression is important because timely recognition and treatment can make a significant difference. In this article, we will discuss its symptoms, causes, and treatment options, while also guiding new mothers and families on when to seek help for postpartum depression.
What is Postpartum Depression?
Postpartum depression is a mood disorder that develops after childbirth. Unlike the short-lived “baby blues,” which usually resolve within two weeks, postpartum depression is more severe and persistent. It can appear any time within the first year after delivery, though it is most common in the first three months.
Medical experts describe postpartum depression as a combination of biological, psychological, and social factors that disrupt a mother’s ability to care for herself and her baby. It is not a sign of weakness or failure but a genuine medical condition requiring attention and support.
Globally, studies suggest that 1 in 7 new mothers may experience postpartum depression. In India, the prevalence is even higher in some regions due to social stressors, cultural expectations, and lack of awareness.
It is also important to note that the term postnatal depression is often used interchangeably with postpartum depression, particularly in the UK and some Asian countries. Both describe the same condition.
Postpartum Depression vs Baby Blues
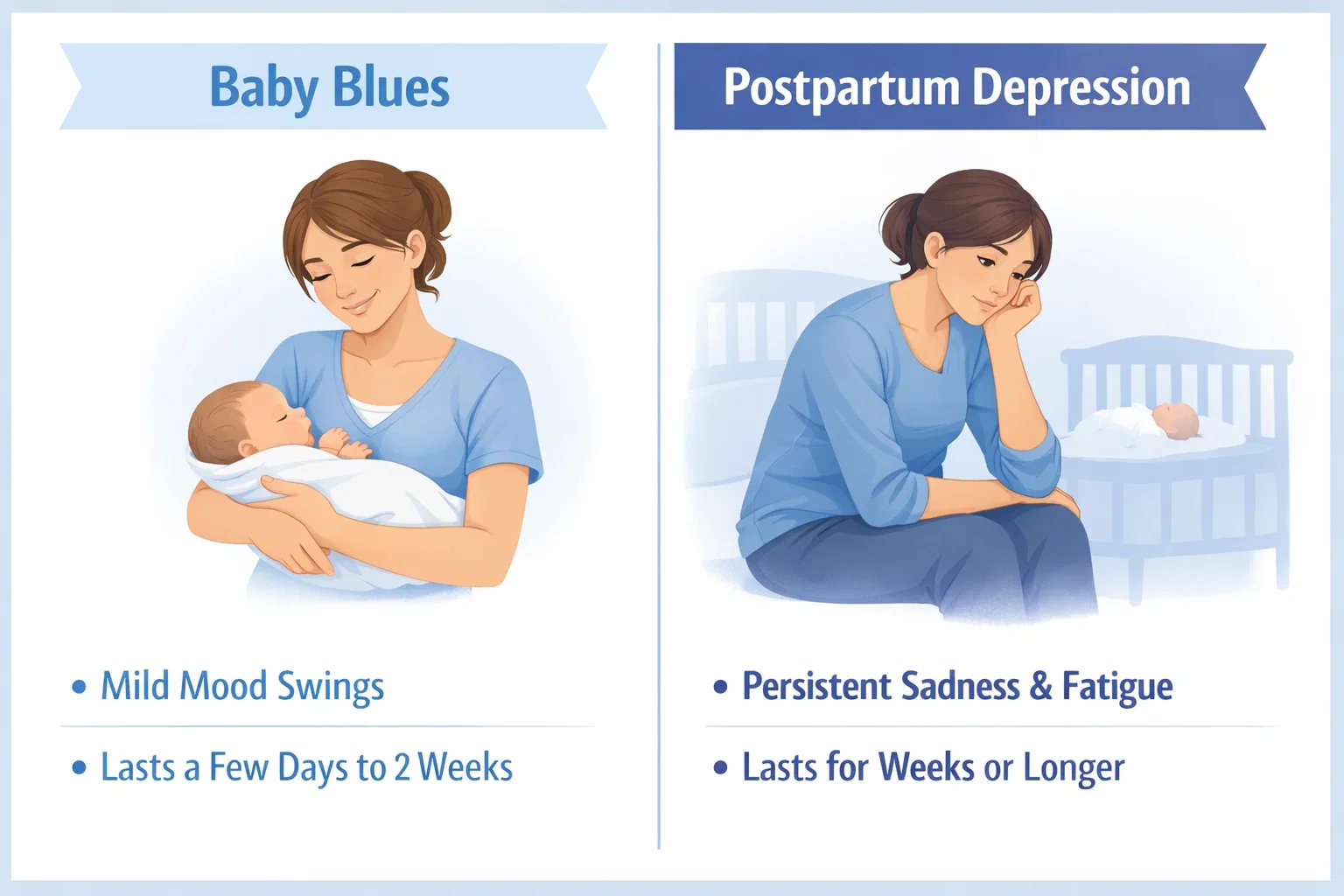
Many new mothers experience emotional ups and downs shortly after childbirth. This common reaction, called the baby blues, affects up to 70–80% of women. The baby blues typically involve mood swings, tearfulness, irritability, or feeling overwhelmed – but these symptoms are mild and usually fade within two weeks without medical intervention.
In contrast, postpartum depression is more severe, longer lasting, and disruptive. It can begin within weeks of delivery or appear later in the postpartum year. Unlike the baby blues, postpartum depression does not simply “go away” with rest or time. Mothers may experience intense sadness, hopelessness, and difficulty bonding with their baby. These symptoms can interfere with day-to-day functioning, relationships, and overall health.
Key Differences Between Baby Blues and Postpartum Depression
| Aspect | Baby Blues | Postpartum Depression |
|---|---|---|
| Onset | Within 2–3 days after delivery | Within weeks to months after delivery |
| Duration | Up to 2 weeks | Several weeks to months; may persist up to a year |
| Symptoms | Mild mood swings, irritability, crying spells | Persistent sadness, anxiety, loss of interest, fatigue, withdrawal |
| Impact | Minimal; daily functioning intact | Significant impairment in caring for self and baby |
| Treatment | Usually resolves on its own | Requires medical evaluation and treatment |
Understanding this difference helps families and caregivers know when to seek help for postpartum depression rather than dismissing symptoms as “normal.”
Causes of Postpartum Depression
There is no single cause of postpartum depression. Instead, it develops from a combination of physical, emotional, and social changes that occur after childbirth. Understanding these risk factors can help families recognize early warning signs and encourage timely intervention.
Biological Factors
- Hormonal shifts: After delivery, estrogen and progesterone levels drop sharply. This sudden change can trigger mood instability and depressive symptoms.
- Genetics and family history: Women with a personal or family history of depression, anxiety, or bipolar disorder are at higher risk.
- Medical complications: Difficult deliveries, cesarean sections, or health issues in the newborn can add physical and emotional strain.
Psychological Factors
- Previous mental health conditions: A history of depression or anxiety increases vulnerability.
- Stress and fatigue: Lack of sleep, constant caregiving, and unrealistic expectations of motherhood contribute significantly.
- Personality traits: Perfectionism, high self-demand, and low coping skills can intensify emotional struggles.
Social and Environmental Factors
- Lack of support: Limited involvement from partners, family, or friends can leave new mothers isolated.
- Financial pressures: Medical expenses, loss of income during maternity leave, or family responsibilities can add stress.
- Cultural expectations: In many cultures, mothers face pressure to “bounce back” quickly or meet traditional caregiving roles, which may increase guilt and shame when struggles arise.
Postpartum depression is rarely the result of a single cause. Instead, it is the interaction of these biological, psychological, and social factors that pushes some women beyond normal stress into a depressive episode. Recognizing these risk factors can help families know when to seek help for postpartum depression before symptoms worsen.
Recognizing Postpartum Depression Symptoms
Spotting postpartum depression symptoms early is crucial for timely diagnosis and treatment. Unlike short-term emotional changes, these symptoms are persistent, intense, and often interfere with a mother’s ability to care for herself and her baby.

Emotional Symptoms
- Persistent sadness, emptiness, or hopelessness
- Intense mood swings or frequent crying spells
- Loss of interest in activities that once brought joy
- Difficulty bonding with the baby or feeling detached
Cognitive and Behavioral Symptoms
- Difficulty concentrating, remembering, or making decisions
- Withdrawal from family and friends
- Overwhelming guilt or feeling like a “bad mother”
- Thoughts of harming oneself or the baby (urgent red flag requiring immediate medical help)
Physical Symptoms
- Chronic fatigue or lack of energy despite rest
- Changes in appetite – eating too little or overeating
- Sleep problems (insomnia, restless sleep, or oversleeping)
- Headaches, stomachaches, or other unexplained pains
Postpartum Anxiety vs Depression
While depression is characterized by sadness and lack of motivation, some women experience more anxiety symptoms after childbirth.
- Postpartum depression → sadness, hopelessness, withdrawal, fatigue.
- Postpartum anxiety → constant worry about the baby’s health or safety, racing thoughts, panic attacks, or obsessive behaviors.
In many cases, mothers may experience both anxiety and depression simultaneously, which can intensify emotional distress.
Recognizing these signs early helps families and caregivers understand when to seek help for postpartum depression rather than waiting for the condition to resolve on its own.
When to Seek Help for Postpartum Depression
Every new mother experiences emotional fluctuations after childbirth, but it is important to know when to seek help for postpartum depression. Timely intervention not only protects the mother’s health but also strengthens her ability to bond with and care for her baby.

Early Warning Signs
You should reach out for professional guidance if symptoms:
- Last longer than two weeks after delivery
- Intensify instead of improving with time
- Interfere with eating, sleeping, or daily functioning
- Create difficulties in caring for the baby
Red Flags Requiring Immediate Medical Attention
- Thoughts of self-harm or harming the baby
- Severe hopelessness or feelings of worthlessness
- Inability to bond with or even look at the baby
- Panic attacks or extreme anxiety episodes
If any of these red flags appear, urgent medical evaluation is essential. Hospitals and clinics have trained professionals who can provide safe, evidence-based treatment.
Role of Family and Friends
Sometimes mothers may not recognize the severity of their symptoms. In such cases, partners, relatives, and friends play a crucial role in encouraging her to seek professional help. Compassionate conversations, offering practical help, and reducing stigma make a major difference.
By recognizing these signs early and acting quickly, families can prevent the progression of depression and begin the path to recovery with medical and emotional support.
Impact of Postpartum Depression on Mother and Baby
Postpartum depression not only affects the mother’s emotional well-being but also has a ripple effect on her baby, partner, and family. Recognizing these consequences highlights the urgency of timely diagnosis and treatment.
Impact on the Mother
- Physical exhaustion: Persistent fatigue and poor sleep can worsen recovery after childbirth.
- Emotional health: Feelings of guilt, worthlessness, and hopelessness may deepen, increasing the risk of chronic depression.
- Daily functioning: Simple tasks like feeding, bathing, or soothing the baby may feel overwhelming, leading to frustration and withdrawal.
Impact on the Baby
- Bonding difficulties: A mother struggling with depression may find it hard to respond to her baby’s emotional cues.
- Developmental delays: Research shows infants of untreated mothers may face challenges in emotional regulation, speech development, or social interaction.
- Feeding and sleep disruptions: Irregular care patterns can impact the baby’s growth and routine.
Impact on the Family
- Partner strain: Fathers or partners may feel helpless or stressed, leading to relationship conflicts.
- Household stress: A tense atmosphere at home can affect older children and overall family harmony.
- Social isolation: Families may withdraw from friends or community due to stigma or lack of understanding.
Addressing postpartum depression early ensures the well-being of both the mother and baby, while also strengthening family bonds. Support from medical professionals, family, and postpartum depression support groups can significantly reduce these impacts.
Postpartum Depression Diagnosis
Timely diagnosis of postpartum depression is essential for effective treatment. Since many new mothers may dismiss their symptoms as “just stress” or confuse them with normal baby blues, healthcare providers rely on structured tools and clinical evaluation to confirm the condition.
Screening Methods and Postpartum Depression Test
- Edinburgh Postnatal Depression Scale (EPDS): A widely used questionnaire that helps assess mood changes and depressive symptoms in new mothers.
- Patient Health Questionnaire (PHQ-9): Another standardized screening tool that evaluates the severity of depression.
- Clinical interviews: Doctors or psychologists may ask about emotional well-being, sleep, appetite, energy levels, and thoughts of self-harm.
These postpartum depression tests are not meant to label mothers negatively but to identify those needing timely support and treatment.
Clinical Evaluation
Diagnosis also involves ruling out medical conditions that can mimic depression, such as thyroid disorders, anemia, or nutritional deficiencies. A detailed history of mental health and family background helps shape a more accurate diagnosis.
Postnatal Depression Terminology
In some countries, especially the UK and parts of Asia, the term postnatal depression is used instead of postpartum depression. Both terms describe the same condition, and healthcare professionals treat them with similar diagnostic standards.
Early diagnosis ensures that treatment can begin before symptoms worsen, improving both the mother’s recovery and the baby’s well-being.
Postpartum Depression Treatment Options
Treatment for postpartum depression depends on the severity of symptoms, overall health, and family circumstances. The good news is that effective therapies are available, and with the right support, most mothers recover fully.
Medical Treatments
- Antidepressant medications: Doctors may prescribe safe options, including some compatible with breastfeeding. These help correct chemical imbalances and lift mood.
- Hormone therapy: In select cases, estrogen-based therapies may be considered, though they require close monitoring.
- Hospital-based care: For severe cases with suicidal thoughts or inability to care for the baby, inpatient or day-care treatment ensures safety and structured recovery.
Therapy Approaches
- Cognitive Behavioral Therapy (CBT): Helps mothers identify negative thought patterns and replace them with healthier coping strategies.
- Interpersonal Therapy (IPT): Focuses on relationships, role transitions, and communication to reduce isolation and conflict.
- Couples or family therapy: Strengthens partner involvement and creates a stronger support system at home.
Lifestyle and Home Remedies
- Rest and sleep: Creating a realistic sleep schedule, even if it means short naps, improves mood and energy.
- Exercise: Light physical activity such as walking or yoga releases endorphins, reducing depressive symptoms.
- Balanced nutrition: Omega-3 fatty acids, lean proteins, and whole grains support brain health and recovery.
- Mindfulness practices: Meditation, journaling, or deep-breathing techniques help manage stress and anxiety.
Family Support and Postpartum Depression Support Groups
- Partner and family involvement: Sharing household tasks, offering reassurance, and encouraging treatment make recovery smoother.
- Support groups: Both in-person and online postpartum depression support groups provide a safe space to share experiences, reduce stigma, and learn coping strategies.
- Community resources: Hospitals, NGOs, and women’s health organizations often provide counseling sessions and group therapy.
Treatment should always be personalized. A combination of medical, therapeutic, and lifestyle measures, along with strong family support, ensures the best chance of recovery.
Postpartum Depression and Recovery Journey
Recovering from postpartum depression is a gradual process that varies from one woman to another. With timely treatment and strong support, most mothers can regain emotional balance and return to enjoying motherhood.

How Long Does Postpartum Depression Last?
- Mild to moderate cases: With therapy and support, recovery often begins within a few months.
- Severe cases: If untreated, postpartum depression can last for a year or longer, and in some cases, evolve into chronic depression.
- With treatment: Women receiving early professional care (medication, therapy, or combined approaches) show significant improvement within 3–6 months.
It’s important to remember that recovery is not linear. Some mothers may feel better quickly, while others experience ups and downs before achieving full stability.
General Recovery Experiences
- Physical health improves once rest, nutrition, and self-care are prioritized.
- Emotional stability returns as therapy and family support reduce guilt, sadness, and anxiety.
- Bonding with the baby strengthens when depressive symptoms fade, improving both mother and child well-being.
- Confidence in parenting grows, helping mothers manage stress and household responsibilities more effectively.
Role of Ongoing Support
Even after symptoms improve, continued check-ins with healthcare providers, participation in postpartum depression support groups, and leaning on family can prevent relapse. Recovery is not just about ending depression – it’s about building resilience for the future.
Mayflower Hospital’s Approach to Postpartum Depression Care
At Mayflower Hospital, we understand that postpartum depression is more than just a medical diagnosis – it is a deeply personal journey that requires compassionate, evidence-based care. Our approach focuses on supporting both the mother and her family at every stage of recovery.
Multidisciplinary Expertise
- Gynecologists and obstetricians monitor physical recovery after childbirth and identify early signs of depression.
- Psychologists and psychiatrists provide therapy and, where necessary, safe medication management.
- Nutritionists and physiotherapists assist with lifestyle interventions such as diet, exercise, and sleep regulation.
Personalized Treatment Plans
Every mother’s experience is unique. Our team designs individualized care plans that may combine counseling, therapy, and medical treatment, ensuring mothers feel supported rather than judged.
Family-Centered Support
Since family involvement is vital to recovery, our programs encourage partners and relatives to participate in therapy sessions and workshops. This ensures mothers receive emotional reinforcement both at home and in the hospital.
Ongoing Guidance and Community Resources
- Access to postpartum depression support groups (both in-person and online)
- Regular follow-ups to track progress and adjust treatment
- Educational sessions to help families understand when to seek help for postpartum depression
By combining medical expertise with compassionate care, Mayflower Hospital helps mothers navigate postpartum depression with confidence, ensuring a healthier future for both mother and baby.
If you or a loved one is experiencing symptoms of postpartum depression, reach out to Mayflower Hospital today for confidential, professional support.
Conclusion
Postpartum depression is a serious but treatable condition that affects many new mothers after childbirth. While emotional ups and downs are normal in the early weeks, persistent sadness, anxiety, or difficulty bonding with the baby are signs that it may be more than the “baby blues.” Recognizing the signs of postpartum depression and understanding when to seek help can make all the difference in recovery.
With timely diagnosis, effective postpartum depression treatment, and strong support from family and professionals, mothers can regain confidence, rebuild emotional balance, and enjoy a healthy relationship with their baby.
At Mayflower Hospital, our team of gynecologists, psychologists, and mental health experts are here to provide compassionate, evidence-based care. Remember, seeking help is not a weakness – it’s the first step toward healing for both mother and child.
If you or someone you know is struggling with symptoms of postpartum depression, contact Mayflower Hospital for confidential guidance and support.
FAQs on Postpartum Depression
Postpartum depression affects about 1 in 7 new mothers globally. In India, studies suggest the prevalence may be higher due to social and cultural pressures, making early recognition and support even more critical.
Baby blues cause mild mood swings, irritability, and crying spells that resolve within two weeks. Postpartum depression, however, lasts longer, is more intense, and interferes with daily life and mother–baby bonding.
Mild cases may improve with lifestyle changes and strong family support. However, most cases require medical evaluation, therapy, or structured support. Ignoring symptoms can prolong recovery.
Yes. Although less common, fathers can develop depression after the birth of a child, often linked to stress, sleep deprivation, or relationship challenges. Professional help can benefit both parents.
Breastfeeding may have protective effects due to hormonal release and bonding benefits. However, difficulties with breastfeeding can also increase stress and trigger depressive symptoms. Each case is unique.
Untreated postpartum depression may last for months or longer, potentially becoming chronic. It can negatively impact the mother’s health, baby’s development, and family well-being. Early treatment leads to better outcomes.
Author
-

Dr. Smeet, true to his name, is known for his warm personality and cheerful smile that make patients instantly feel at ease with him.
Until now, he has performed 8000+ surgeries and several of which are supra-major surgeries for deep infiltrating endometriosis and fertility enhancing surgeries. With several publications in notable journals, he is constantly pushing the envelope of possibilities in gynecological surgeries