Endometriosis management is essential for women who experience persistent pelvic pain, fatigue, and difficulty maintaining their daily rhythm. For many, the condition doesn’t just affect physical health – it impacts energy levels, focus, and emotional well-being. Balancing personal care with professional responsibilities often becomes an everyday challenge, especially when chronic discomfort interferes with productivity.
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, leading to inflammation, pain, and sometimes fertility issues. While there’s no one-size-fits-all cure, proactive management through medical treatment, nutrition, and lifestyle adjustments can help women regain control over their lives. Understanding how endometriosis influences both the body and the mind is the first step toward living comfortably and working efficiently despite the symptoms.
At Mayflower Hospital, our specialists emphasize a holistic approach – combining expert medical care with personalized strategies that empower women to handle work-life demands with confidence. This guide explores practical ways to manage pain, reduce fatigue, and maintain workplace productivity while living with endometriosis.
Understanding Endometriosis and Its Impact on Daily Life
Living with endometriosis often means managing unpredictable pain and chronic fatigue that can disrupt even simple daily routines. Some days, the discomfort is tolerable; on others, it may hinder focus, energy, or mobility. Effective endometriosis management begins with recognizing how these symptoms manifest and influence both personal well-being and work performance.
What Endometriosis Is and Why It Needs Ongoing Management
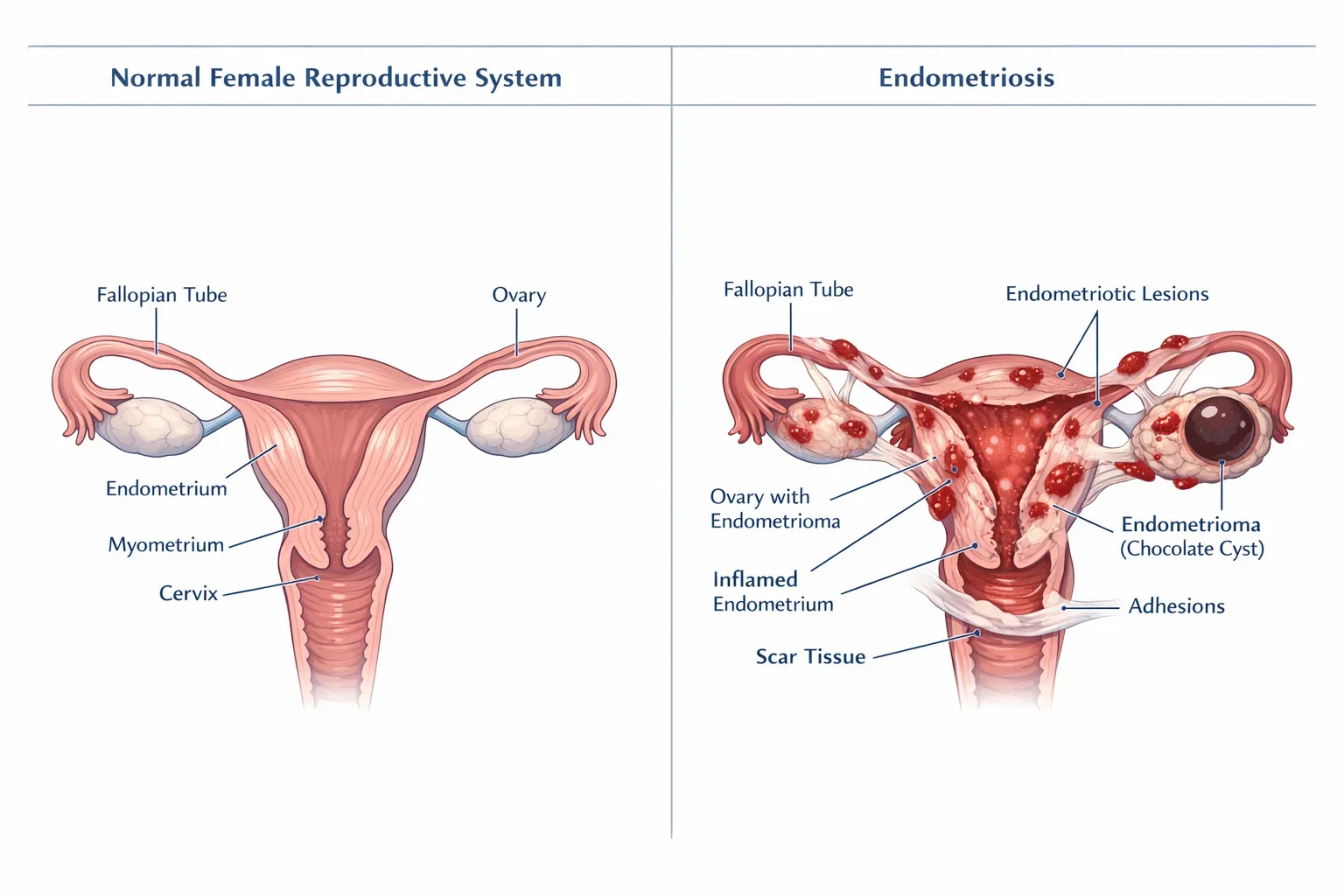
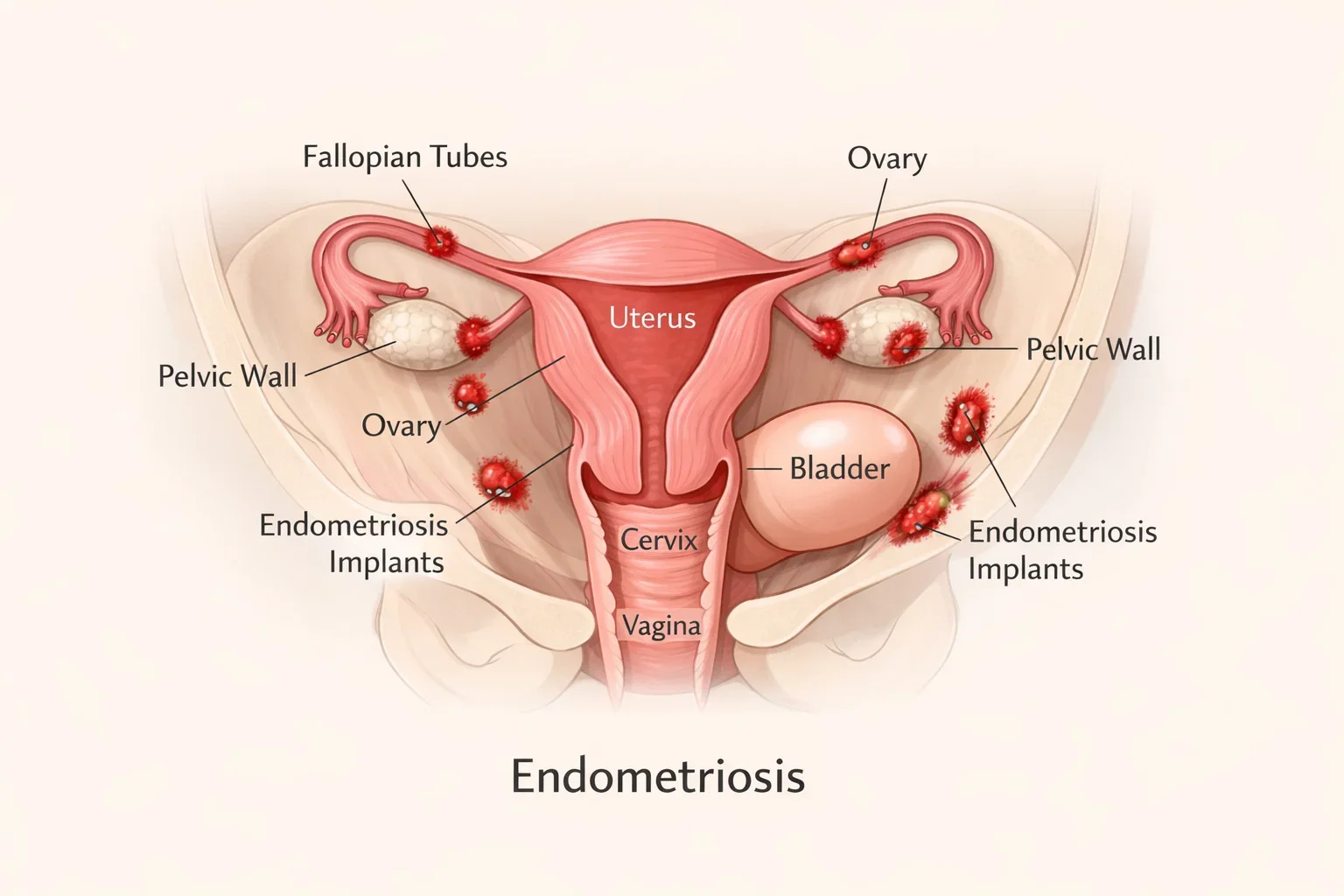
Endometriosis is a chronic condition where endometrial-like tissue grows outside the uterus, commonly on the ovaries, fallopian tubes, or pelvic lining. This misplaced tissue behaves as it would inside the uterus – thickening, breaking down, and bleeding with each menstrual cycle – but without an exit path, it causes inflammation and scarring.
Over time, this can result in pelvic pain, bloating, and other complications that make daily activities challenging. Because symptoms vary in severity, long-term management focuses on symptom control and prevention of recurrence rather than a one-time treatment.
Common Symptoms and Hidden Challenges Women Face
While the most recognized symptom is pelvic pain, many women experience a wide range of issues such as fatigue, digestive discomfort, back pain, and emotional stress. The hidden challenge lies in how these symptoms affect routine tasks. Standing for long hours, attending meetings, or maintaining focus through pain can quickly lead to exhaustion.
Women often push through discomfort to maintain productivity, yet untreated chronic pain may result in reduced efficiency and burnout. Acknowledging these limitations is not a sign of weakness but the foundation of effective management.
How Chronic Pain and Fatigue Affect Productivity and Mental Health
Persistent pain and endometriosis fatigue can diminish motivation and focus, directly affecting professional output. Many women describe a mental fog that makes concentration difficult. Emotional strain – including anxiety or guilt over decreased performance – often adds to the challenge.
Comprehensive endometriosis management involves addressing both physical and psychological aspects. Supportive workplace measures, rest planning, and medical consultation can help restore balance, making it possible to perform effectively without compromising health.
The Connection Between Endometriosis and Work Productivity
Women with endometriosis often describe their workdays as a constant balancing act – juggling deadlines, meetings, and pain management. While determination helps, chronic symptoms can gradually wear down physical stamina and mental focus. Understanding how endometriosis at work affects productivity is essential not only for those managing the condition but also for employers seeking to create more inclusive, health-aware workplaces.
For many professionals, the biggest challenge isn’t the diagnosis itself – it’s maintaining consistency in the face of chronic pain, fatigue, and emotional strain. By identifying workplace triggers and making small but impactful adjustments, women can reclaim control and continue thriving in their careers.
Working with Endometriosis – Real-Life Struggles Women Encounter
Everyday professional life becomes unpredictable when pain or fatigue fluctuates. Tasks that require concentration or long periods of sitting can intensify discomfort, while stress from tight schedules may aggravate symptoms further. Many women also find themselves hesitant to disclose their condition, fearing judgment or reduced opportunities.
These challenges highlight why working with endometriosis requires compassion – both self-compassion and understanding from peers or managers. Setting realistic expectations, communicating needs clearly, and pacing workloads can prevent burnout. Small adjustments like flexible schedules, comfortable seating, or access to rest periods can make a remarkable difference.
Managing Chronic Pain and Fatigue While Meeting Deadlines
Balancing productivity with persistent symptoms demands structured time management and honest self-awareness. Creating a daily rhythm that accommodates energy fluctuations helps minimize fatigue. Prioritizing tasks that require maximum focus during high-energy hours and scheduling breaks during pain flare-ups can preserve productivity.
Using ergonomic furniture, staying hydrated, and incorporating light stretching can help manage chronic pain at work. For severe pain, discussing medical options for endometriosis pain relief with a gynecologist can prevent physical exhaustion from escalating.

How Workplaces Can Support Employees Living with Endometriosis
A supportive workplace can play a major role in long-term chronic pain management. Simple accommodations – such as adjustable desks, quiet spaces, or flexible working hours – empower employees to stay productive without worsening their symptoms.
Managers and HR teams should also be educated about invisible illnesses like endometriosis to foster a culture of understanding. When employees feel safe sharing their challenges, it becomes easier to access help without fear of stigma or reduced credibility. Such openness encourages a healthier, more empathetic work environment.
Coping with Chronic Pain at Work – Emotional and Social Aspects
Endometriosis doesn’t only affect the body; it influences emotions and social confidence as well. Feeling misunderstood or pressured to “push through” pain can create frustration and anxiety. Supportive colleagues and open conversations can make daily routines less isolating.
Employers who promote mental health awareness, provide counselling options, or allow flexible leave for medical care create an atmosphere where employees can truly thrive. This sense of belonging is as important as medical management itself.
Addressing the physical and emotional toll of endometriosis at work is just the beginning. Long-term success depends on proactive management – from medical treatments to holistic lifestyle habits that promote healing. In the next section, we explore effective pain relief, nutrition, and stress-control strategies that help women live and work comfortably.
Effective Endometriosis Management Strategies
Successfully managing endometriosis requires more than pain medication or occasional rest – it’s about creating a balanced plan that supports both physical and emotional health. Whether you’re dealing with recurring pelvic pain, chronic fatigue, or the pressure of staying productive at work, combining medical guidance with daily wellness habits can make a significant difference.
Below are evidence-based strategies designed to improve comfort, reduce symptom intensity, and enhance your overall quality of life.
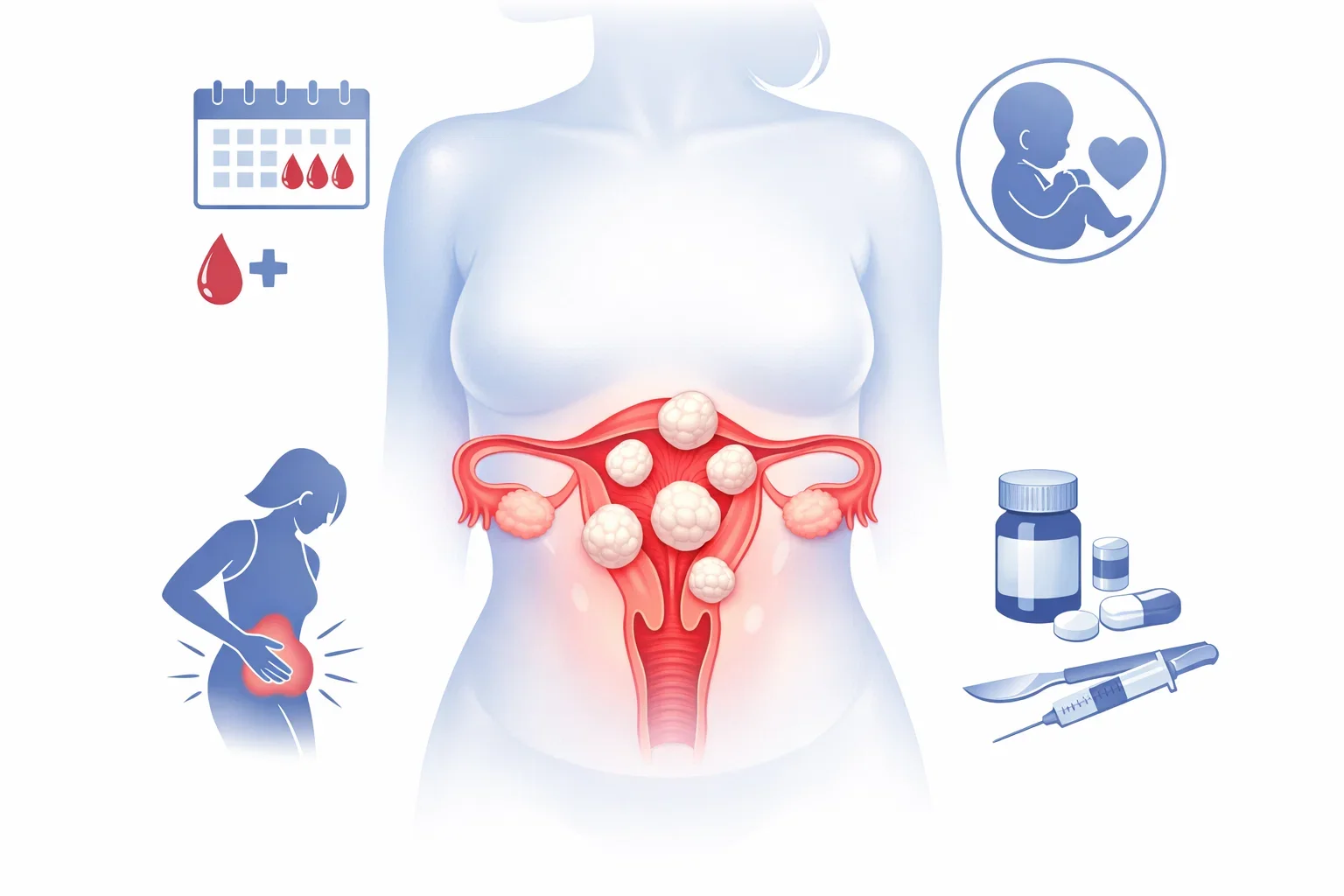
Medical Treatments and Pain Relief Options for Endometriosis
Effective medical management of endometriosis is central to long-term relief and quality of life. It focuses on controlling inflammation, regulating hormones, and easing pain so women can function comfortably at work and home. Depending on the severity of your symptoms, your gynecologist may recommend:
- Hormonal therapy: Birth control pills, hormonal IUDs, or GnRH agonists help reduce or stop menstruation, preventing further growth of endometrial tissue.
- Pain medication: Over-the-counter anti-inflammatories like ibuprofen can relieve discomfort, but persistent pain may require prescription options.
- Laparoscopic surgery: For those with severe pain or fertility complications, minimally invasive surgery helps remove lesions and scar tissue.
For many women, the medical management of endometriosis combines hormonal therapy, nonsteroidal anti-inflammatory medications, and supportive lifestyle changes. This integrated approach helps reduce symptom frequency and prevents the condition from progressing. Regular monitoring and communication with your specialist ensure that the treatment remains effective as your body’s needs evolve.
Post-surgery recovery and symptom control require continuous endometriosis management, including regular follow-ups and lifestyle adjustments. Consulting specialists at Mayflower Hospital’s Endometriosis Centre ensures that treatment plans are tailored to your personal needs and long-term health goals.
Pelvic Pain Relief Exercises and Gentle Movement Routines
Movement might feel counterintuitive during pain episodes, but gentle exercise often helps relieve pelvic tightness and improves blood circulation. Activities like yoga, walking, or light stretching can relax tense muscles and ease inflammation.
Some recommended options include:
- Pelvic tilts or bridges to strengthen core muscles.
- Restorative yoga poses (like child’s pose or supine twist) for tension release.
- Breathing exercises to reduce stress-related pain.
A physiotherapist experienced in women’s health can help design a personalized movement routine. The goal isn’t intensity – it’s consistency. Gradual, mindful activity promotes long-term resilience and supports overall chronic pain management.
Lifestyle Modifications – Diet, Rest, and Energy Conservation
A well-structured lifestyle can dramatically reduce symptom severity. Prioritize:
- Balanced nutrition: Anti-inflammatory foods such as leafy greens, berries, and omega-3-rich fish help reduce pain flare-ups.
- Sleep hygiene: Aim for 7–8 hours of quality rest. Poor sleep worsens fatigue and pain perception.
- Energy pacing: Plan your day around energy highs and lows. Alternate intense tasks with lighter ones to manage chronic fatigue productivity effectively.

Small changes like standing up every hour, using a heat compress, or practicing short meditation breaks during work can also relieve pelvic tension and stress.
Mindfulness, Stress Management, and Mental Health Care
Emotional well-being plays a major role in living with endometriosis. Chronic pain can heighten stress hormones, making symptoms worse. Mind-body techniques help counter this cycle:
- Meditation and breathing exercises lower anxiety and promote calm.
- Cognitive-behavioral therapy (CBT) helps build coping skills for pain perception.
- Support groups offer connections with others facing similar challenges.
Integrating mindfulness into your daily routine doesn’t just reduce pain; it improves focus, patience, and emotional strength – all essential for maintaining work-life balance.
Pain control and emotional care are central to healing, but nutrition is equally vital. The right foods can reduce inflammation, ease cramps, and boost stamina – especially for those managing endometriosis fatigue. In the next section, we’ll explore dietary choices that support your recovery and daily energy.
Nutrition and Endometriosis Management – Eating for Healing and Energy
Nutrition plays a powerful role in endometriosis management. The foods you eat can influence inflammation levels, hormonal balance, and overall energy – all key factors in reducing pain and fatigue. A mindful diet helps control flare-ups, supports digestion, and provides sustained stamina for work and daily life.
Instead of following restrictive fads, focus on balanced, anti-inflammatory nutrition that nourishes the body and supports recovery from within.
Anti-Inflammatory Foods to Reduce Pain and Bloating
Chronic inflammation is one of the key drivers of pelvic pain and fatigue in endometriosis. Incorporating anti-inflammatory foods can make a noticeable difference in symptom control. Some of the most beneficial include:
- Leafy greens: Spinach, kale, and broccoli are rich in antioxidants and magnesium, which may help reduce cramps.
- Fatty fish: Salmon, sardines, and mackerel provide omega-3 fatty acids that help lower inflammation.
- Colorful fruits: Berries, oranges, and cherries offer natural antioxidants to fight oxidative stress.
- Turmeric and ginger: Both have anti-inflammatory properties that ease pain and bloating.
Hydration is equally important. Drinking enough water throughout the day helps minimize bloating and fatigue, supporting better concentration at work.
Diet Tips for Reducing Endometriosis Fatigue
Persistent tiredness, or endometriosis fatigue, can often be linked to nutrient deficiencies, poor sleep, or blood sugar fluctuations. To manage energy effectively:
- Eat smaller, balanced meals every 3–4 hours to maintain steady glucose levels.
- Prioritize iron-rich foods such as lentils, spinach, and pumpkin seeds to prevent anemia caused by heavy bleeding.
- Add complex carbohydrates like oats, quinoa, and sweet potatoes for slow energy release.
- Don’t skip breakfast – it sets the metabolic tone for your workday.
Combining these choices with regular hydration can help stabilize mood, prevent afternoon energy crashes, and improve chronic fatigue productivity.
What to Avoid – Trigger Foods and Processed Items
Just as some foods help manage pain, others can trigger inflammation and worsen discomfort. Women with endometriosis often find relief by limiting or avoiding:
- Processed meats and high-fat dairy, which can raise estrogen levels.
- Refined sugars and caffeine, which cause hormonal fluctuations and bloating.
- Gluten and trans fats, which may increase inflammation in some individuals.
- Alcohol, as it can interfere with liver function and hormone metabolism.
Keeping a food diary helps identify personal triggers. Small dietary adjustments, made consistently, can lead to long-term improvement in symptom intensity.
A balanced diet not only supports physical recovery but also enhances energy, mental clarity, and emotional resilience. However, effective endometriosis management extends beyond nutrition. Learning how to rest, recharge, and pace yourself after long workdays is equally essential. The next section focuses on managing chronic pain and fatigue beyond workplace routines.
Managing Chronic Pain and Fatigue Beyond Work Hours
Endometriosis doesn’t stop affecting your life once you leave the office. Evenings and weekends often bring waves of pelvic pain or exhaustion that make recovery difficult. To truly improve quality of life, you need strategies that go beyond symptom control – methods that restore your body’s energy reserves, regulate sleep, and strengthen your emotional resilience. Effective endometriosis management means treating rest and recovery as essential, not optional.
How to Balance Rest and Routine
Finding the right balance between activity and rest is crucial for women dealing with chronic pain. Total inactivity can lead to stiffness, while overexertion can worsen fatigue and discomfort. Instead, aim for a structured balance:
- Plan recovery periods after demanding tasks or workdays.
- Schedule gentle stretching or short walks to promote circulation.
- Use heat therapy – such as warm baths or heating pads – to relax muscles before sleep.
Rather than pushing through pain, acknowledge your body’s signals. Taking small breaks when symptoms flare up helps prevent long-term exhaustion and supports steady productivity.
Creating a Sleep and Recovery Plan for Better Energy
Sleep quality has a direct impact on hormone balance, mood, and pain perception. Many women with endometriosis experience insomnia or disrupted sleep due to discomfort. Improving nighttime recovery can drastically reduce fatigue and emotional strain.
Try these evidence-based strategies:
- Maintain a consistent bedtime routine – go to bed and wake up at the same time daily.
- Limit screen exposure before sleep to avoid overstimulation.
- Use supportive pillows or sleep in positions that relieve pelvic tension.
- Practice deep breathing or guided relaxation to calm the nervous system.
Even small improvements in sleep quality can enhance daytime focus and reduce reliance on stimulants like caffeine, which often aggravate symptoms.
When to Seek Professional Help from an Endometriosis Specialist
If pain and fatigue persist despite lifestyle changes, it may be time to consult a specialist. Endometriosis fatigue or recurring pain that interferes with daily activities could indicate deeper tissue involvement that requires medical attention.
A gynecologist specializing in endometriosis can assess your symptoms, recommend advanced therapies, or suggest surgical interventions if necessary. At Mayflower Hospital, our specialists, including Dr. Sanjay Patel, focus on minimally invasive procedures and holistic aftercare to ensure long-term recovery and comfort.
In some cases, your doctor may recommend a comprehensive plan for the medical management of endometriosis before considering surgery. This can include hormonal treatments, pain-control medication, and physiotherapy-based support designed to stabilize symptoms while maintaining your quality of life.
Physical recovery is vital, but managing endometriosis also requires emotional balance. Chronic pain often leads to stress, anxiety, or even depression – all of which can worsen physical symptoms. The next section explores how emotional well-being and psychological support are integral to comprehensive endometriosis management.
Emotional Health and Coping with Endometriosis
Endometriosis doesn’t only affect the body – it deeply influences mental and emotional well-being. Living with unpredictable pain, fatigue, and medical uncertainty can lead to frustration, anxiety, or even depression. Many women describe feeling “trapped” in their own bodies, especially when they are expected to perform at work or home without acknowledgment of their pain.
Comprehensive endometriosis management must therefore include emotional care. Addressing the mental burden of chronic illness not only improves overall resilience but can also reduce the intensity of physical symptoms by calming the nervous system and lowering stress hormones.
The Psychological Toll of Chronic Pain
Chronic pain can gradually change how the brain processes stress and emotion. Constant discomfort keeps the body in a heightened state of tension, leading to irritability, poor concentration, and sleep disruption. Over time, this cycle can cause emotional burnout.
Recognizing this link is the first step to healing. Emotional exhaustion is not a personal weakness – it’s a physiological response to ongoing strain. Seeking timely psychological support can help you rebuild focus and mental energy while improving your ability to cope with daily challenges.
How Therapy and Support Groups Can Help
Talking about your experiences with chronic pain in a safe space can be incredibly liberating. Individual therapy, particularly cognitive-behavioral therapy (CBT), helps identify negative thought patterns and replaces them with practical coping strategies.
Support groups, whether in-person or online, also provide comfort through shared experiences. Listening to others who have managed similar symptoms or work-life challenges builds a sense of community and validation. Hospitals like Mayflower Women’s Hospital encourage this support-oriented approach, helping patients connect with specialized counsellors and women’s health networks.
Managing Anxiety and Depression Linked to Endometriosis
Emotional symptoms such as anxiety, hopelessness, or withdrawal are common in women dealing with endometriosis at work or in daily life. Constant pain or social misunderstanding can amplify these feelings. Techniques to manage these emotions include:
- Mindfulness meditation: Focused breathing and grounding exercises help regulate thoughts during pain episodes.
- Journaling: Tracking moods and pain patterns offers insight into triggers and progress.
- Creative expression: Art, music, or gentle hobbies can provide emotional release and distraction.
- Professional counselling: A therapist specializing in chronic illness can teach long-term emotional resilience techniques.
These steps, combined with medical treatment, form the foundation of whole-body healing. Caring for your emotional health doesn’t just make life more manageable – it improves physical outcomes too.
Managing your emotional well-being helps you regain stability and confidence, but inspiration from others can be equally healing. In the next section, we’ll share stories of women who have successfully managed their symptoms, rebuilt their careers, and rediscovered balance through effective endometriosis management.
Living with Endometriosis – Stories of Strength and Success
Every woman’s journey with endometriosis is unique – yet the courage to overcome its challenges connects them all. Living with endometriosis often means learning to adapt, set boundaries, and redefine strength. By sharing stories of recovery and perseverance, we highlight the possibility of thriving despite pain, fatigue, and uncertainty. These success stories offer hope and show that effective endometriosis management can help women lead fulfilling personal and professional lives.
Stories from Women Who Found Relief and Balance
For many working professionals, the hardest part is acknowledging that pain doesn’t have to be constant.
Take Neha, a 33-year-old graphic designer who used to struggle with severe pelvic pain that made sitting for long hours unbearable. After consulting an endometriosis specialist, she followed a comprehensive plan involving medication, dietary changes, and gentle yoga. Within months, her symptoms became manageable, and she regained her energy and creativity at work.
Another patient, Aditi, faced recurring fatigue that made it hard to keep up with teaching. She began documenting her symptoms, switched to an anti-inflammatory diet, and adopted short mindfulness sessions before class. These lifestyle changes, supported by professional guidance, helped her regain control over her routine.
Such experiences highlight how individualized treatment – when combined with awareness and self-care – can transform everyday life.
How Personalized Care at Mayflower Improved Their Daily Lives
At Mayflower Women’s Hospital, specialists approach every endometriosis case with personalized precision. Each treatment plan begins with a detailed evaluation to identify symptom triggers and pain patterns. From there, the care team develops a tailored approach that integrates medical treatment, physiotherapy, and emotional support.
Patients frequently report not only reduced pelvic pain but also improved sleep, energy, and mental focus – allowing them to return to work, pursue hobbies, and strengthen relationships.
The hospital’s holistic model – combining advanced laparoscopic techniques with compassionate aftercare – ensures that patients receive continuous guidance throughout their recovery. Many women express that the real success lies not just in reduced pain but in rediscovering confidence and control over their own bodies.
Every story reinforces the same message – endometriosis does not define your capabilities. With proper treatment, awareness, and support, women can continue to live productively and joyfully. The next section provides a practical checklist summarizing everything you need to maintain steady progress in your endometriosis management journey.
Step-by-Step Checklist for Effective Endometriosis Management
Consistency is key when it comes to endometriosis management. While medical treatment forms the foundation, everyday actions determine how effectively you can control pain, prevent flare-ups, and sustain productivity at work and home. This step-by-step checklist brings together practical routines, lifestyle habits, and self-care principles that empower you to manage symptoms confidently.
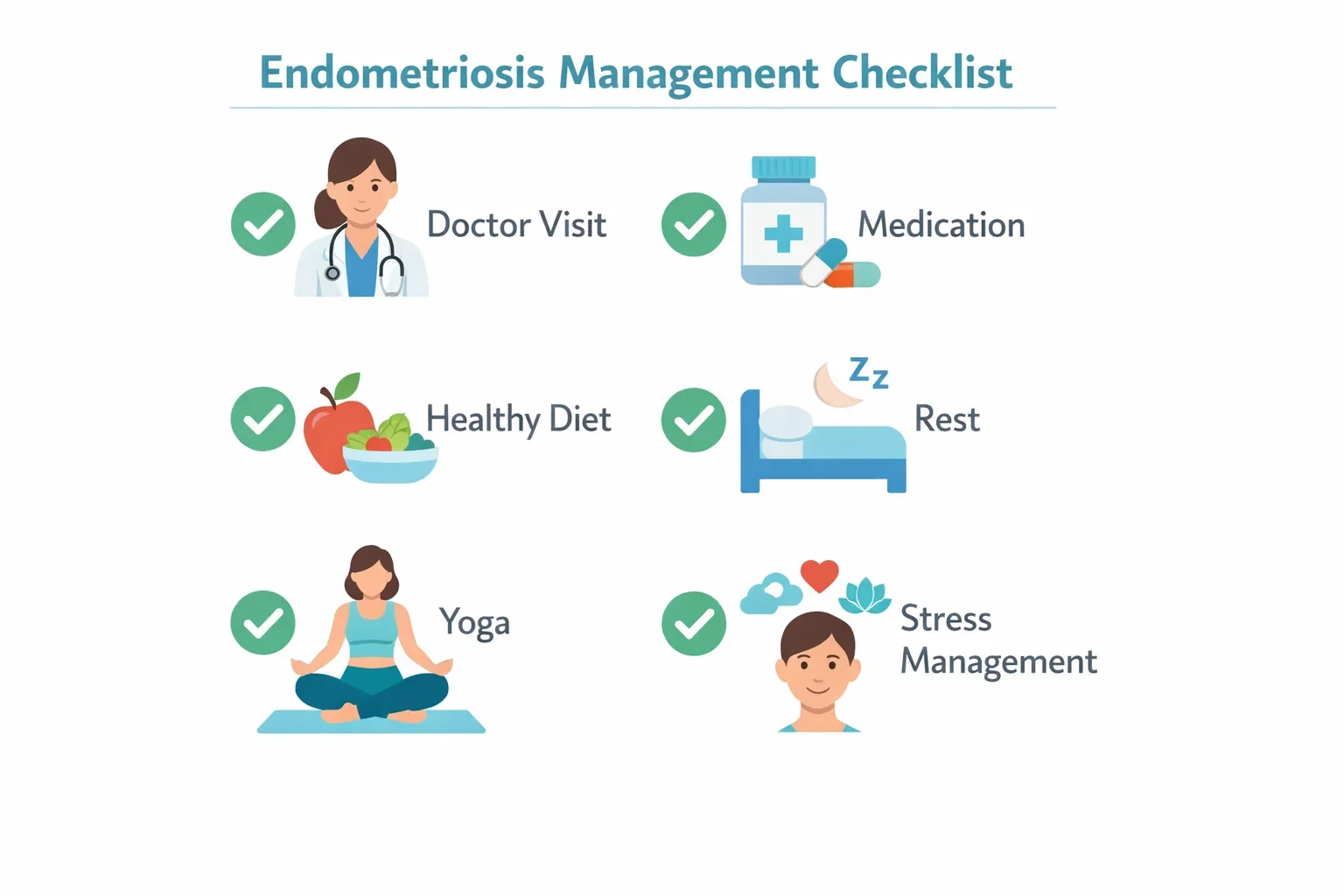
1. Maintain Regular Doctor Consultations
Routine check-ups with an endometriosis specialist help track progress, adjust medication, and prevent complications. Early intervention can stop minor symptoms from developing into severe pain.
2. Keep a Symptom and Pain Journal
Documenting your daily pain levels, fatigue, and diet patterns helps identify what triggers flare-ups. Over time, this data becomes invaluable for your gynecologist when refining your treatment plan.
3. Use Heat Therapy and Ergonomic Support at Work
Heating pads, warm compresses, or ergonomic seating can relieve pelvic pain during long office hours. Consider setting reminders to stand, stretch, or walk briefly every hour to improve circulation and ease muscle stiffness.
4. Follow a Balanced Anti-Inflammatory Diet
Nutrition plays a powerful role in managing inflammation and energy levels. Include omega-3-rich foods, leafy greens, and fresh fruits while avoiding refined sugars, caffeine, and processed items. Staying hydrated is equally important for digestion and fatigue control.
5. Incorporate Gentle Exercise and Stress Management
Low-impact activities such as yoga, walking, or swimming enhance blood flow and reduce discomfort. Pair these with mindfulness or breathing exercises to regulate stress – a known trigger for chronic pain flare-ups.
6. Build a Supportive Workplace Communication Plan
If pain or fatigue interfere with your routine, communicate openly with supervisors or HR. A flexible work schedule, short breaks, or remote work options can significantly ease the pressure of managing endometriosis at work.
If your symptoms persist or begin to interfere with work or personal life, don’t ignore them. The Mayflower Endometriosis Care Team offers expert-led consultation, advanced diagnostics, and minimally invasive treatment options to help you live comfortably and productively.
Book your personalized consultation today and take the first step toward a pain-free, balanced life.
With the right balance of professional care, nutrition, and self-awareness, managing endometriosis becomes achievable and sustainable. To address common questions many women have during this process, the following section offers concise expert-backed answers.
Conclusion – Managing Endometriosis Means Reclaiming Control of Your Life
Living with endometriosis may feel overwhelming at times, but with the right endometriosis management plan, life can be both productive and fulfilling. Pain and fatigue don’t have to define your daily routine or limit your career aspirations. Through a combination of professional medical care, mindful nutrition, balanced rest, and emotional resilience, it’s possible to build a healthier rhythm that supports both your physical and mental well-being.
At Mayflower Women’s Hospital, our specialists believe in a holistic, patient-centered approach. From diagnosis to advanced laparoscopic endometriosis surgery, from pain relief programs to emotional support, every aspect of care is tailored to your unique needs. Our goal is not only to treat symptoms but to help you regain control over your life – one step at a time.
If you’ve been struggling with chronic pain, fatigue, or difficulty balancing work and health, it may be time to seek expert guidance. A consultation with an experienced endometriosis specialist can help you identify the right treatment and lifestyle plan for long-term relief.
Take charge of your well-being – schedule a consultation with Mayflower Hospital’s Endometriosis Care Team today and begin your journey toward a pain-free, empowered life.
FAQs
Women living with endometriosis often have practical questions about daily care, symptom relief, and long-term treatment options. Here are some expert-backed answers to the most common queries related to endometriosis management, designed to help you make informed and confident decisions about your health.
Managing endometriosis pain relief at work starts with preparation and flexibility. Keep a small heating pad or warm compress handy, take short standing or stretching breaks every hour, and stay hydrated. Planning tasks around your energy levels helps balance productivity and comfort. For persistent pain, discuss medical options or hormonal treatments with your gynecologist.
Yes. Endometriosis fatigue can make it hard to stay focused or meet deadlines, especially during flare-ups. Managing your schedule to include breaks, eating iron-rich meals, and getting 7–8 hours of quality sleep are crucial. Learning to pace yourself and set realistic goals ensures long-term productivity without burnout.
Natural pelvic pain relief methods include warm baths, gentle yoga, breathing exercises, and anti-inflammatory foods like turmeric, leafy greens, and salmon. Avoiding processed foods, caffeine, and alcohol can also help minimize inflammation and pain intensity.
Absolutely. A diet rich in fiber, omega-3 fats, and antioxidants helps regulate hormones and reduce inflammation, leading to fewer pain episodes. On the other hand, processed and high-fat foods may worsen symptoms. Consistency in dietary habits often brings visible improvements within a few months.
If pain or fatigue interferes with your daily tasks, disrupts sleep, or affects your work performance, it’s time to consult an endometriosis specialist. Early diagnosis and intervention can prevent further complications and improve your quality of life significantly.
Yes, many women can live a normal, fulfilling life with endometriosis through consistent endometriosis management. While symptoms like pain and fatigue may fluctuate, the right combination of medical care, nutrition, exercise, and stress control can significantly improve comfort and energy. Early diagnosis, regular follow-ups, and support from an endometriosis specialist make it possible to maintain work productivity, relationships, and overall well-being.
Author
-

Dr. Smeet, true to his name, is known for his warm personality and cheerful smile that make patients instantly feel at ease with him.
Until now, he has performed 8000+ surgeries and several of which are supra-major surgeries for deep infiltrating endometriosis and fertility enhancing surgeries. With several publications in notable journals, he is constantly pushing the envelope of possibilities in gynecological surgeries