Endometriosis treatment options are crucial for relieving pain, improving fertility, and restoring everyday comfort. Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, leading to chronic pelvic pain, fatigue, and sometimes infertility. For many women, deciding between medication and surgery can feel overwhelming – but understanding how each works helps make a confident, informed choice.
At Mayflower Women’s Hospital, every treatment plan is personalized. Some patients respond well to non-surgical treatment for endometriosis, including hormonal therapy, pain management, and lifestyle changes. Others may need laparoscopic surgery to remove endometrial lesions or restore fertility. The decision depends on several factors: disease stage, symptom severity, reproductive goals, and tolerance to medications.
Diagnosis plays a critical role before choosing the right treatment. At Mayflower, each care plan begins with a Pelvic MRI for Endometriosis Diagnosis, which maps lesion depth, adhesions, and organ involvement. This ensures your specialist can recommend the most effective medical or surgical approach for lasting results.
In this blog, you’ll discover how both medication and surgery compare – their effectiveness, recovery timelines, risks, and costs – helping you take informed steps toward better health, comfort, and peace of mind.
Understanding Endometriosis and Its Impact on Daily Life
Endometriosis is more than just a painful period – it’s a chronic condition that can affect nearly every part of a woman’s life. The disease occurs when tissue similar to the uterine lining grows outside the uterus, on organs such as the ovaries, fallopian tubes, and pelvic walls. These misplaced tissues respond to hormonal changes during each menstrual cycle, leading to inflammation, scarring, and severe pain.
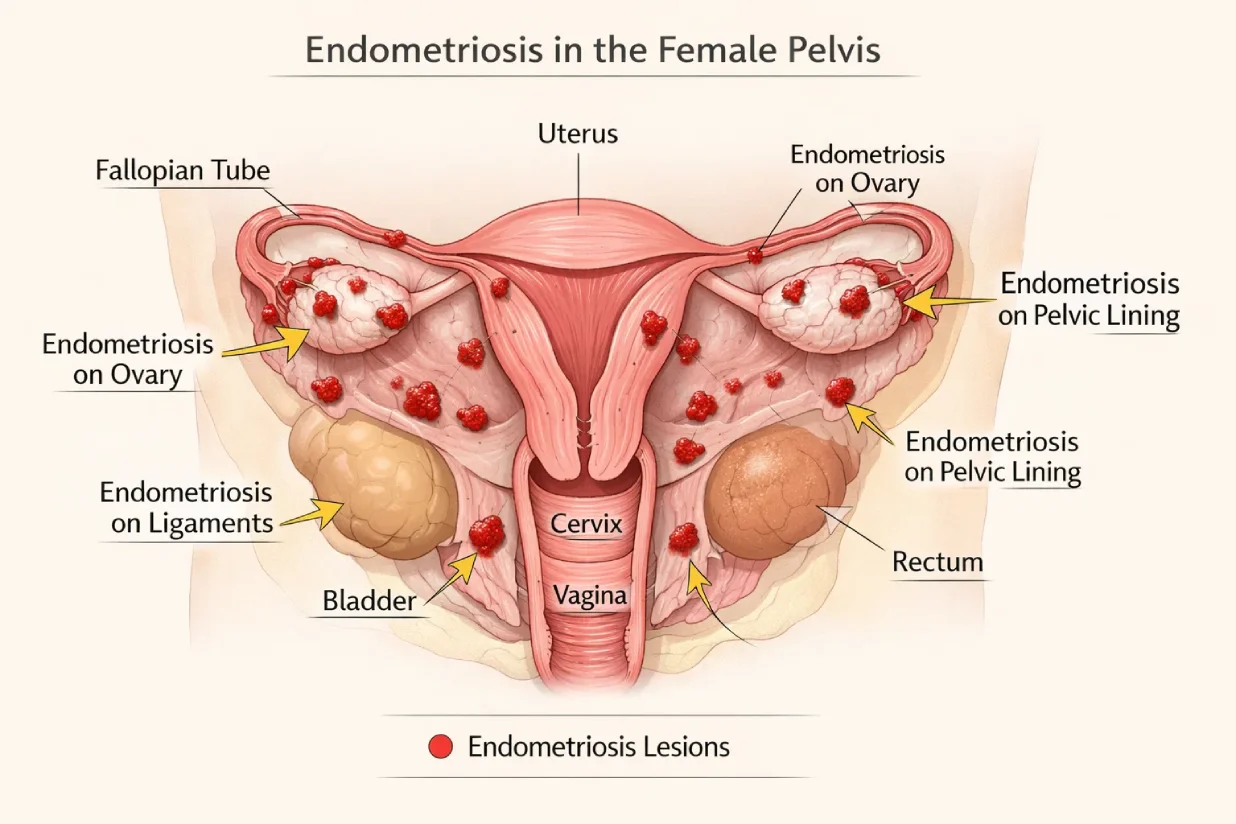
Women with endometriosis often experience persistent pelvic pain, painful intercourse, heavy bleeding, bloating, fatigue, and sometimes infertility. The emotional toll can be equally significant – many struggle with anxiety, loss of productivity, and social withdrawal due to recurring discomfort. Over time, untreated endometriosis can lead to adhesions and cysts, further complicating reproductive health.
Understanding the impact of endometriosis helps underline why early diagnosis and proper management are essential. Timely intervention can slow the progression, preserve fertility, and improve daily functioning. Specialists now recognize that treatment must go beyond pain relief; it should also target hormonal balance, organ protection, and long-term quality of life.
For many patients, acknowledging symptoms early and seeking medical evaluation – especially through advanced diagnostic tools like pelvic MRI – makes a crucial difference in achieving faster relief and better outcomes.
How Is Endometriosis Treated?
The goal of treating endometriosis is not just to relieve pain but to manage long-term symptoms, preserve fertility, and prevent recurrence. Since the condition behaves differently in every woman, treatment plans are personalized based on factors like age, symptom severity, lesion depth, and future pregnancy goals.
Doctors typically recommend one or a combination of three primary approaches – non-surgical management, medical (hormonal) therapy, and surgical treatment. The choice depends on how far the disease has progressed and how it affects your daily life.
Non-surgical treatment for endometriosis usually begins with pain relief medications and lifestyle modifications. Hormonal therapies are introduced to suppress estrogen production, helping slow the growth of endometrial tissue and reduce inflammation. These options are often suitable for women in the early stages of the condition or those trying to delay surgery.
In more advanced cases, laparoscopic surgery becomes a preferred option, especially when cysts, adhesions, or organ involvement are detected. This minimally invasive procedure allows surgeons to both diagnose and remove endometrial lesions, offering long-lasting symptom relief and improved fertility outcomes.
For many patients, a combination approach works best – using medication to stabilize hormonal levels before or after surgery to minimize recurrence.
Understanding the full range of endometriosis treatment options helps women and their doctors create a structured plan that aligns with both medical needs and lifestyle goals.
Medical Management of Endometriosis (Non-Surgical Options)
Managing endometriosis medically is often the first step before considering surgery, especially for women with mild to moderate symptoms. The goal of medical management is to reduce pain, control hormonal fluctuations, and prevent the growth of endometrial tissue. For many patients, these treatments can significantly improve quality of life without the need for invasive procedures.
Hormonal Therapy for Endometriosis
Hormonal therapy remains one of the most effective non-surgical treatments for endometriosis. Since the condition is estrogen-dependent, controlling hormone levels helps slow tissue growth and reduce inflammation. Common options include:
- Combined oral contraceptives: Help regulate periods and lower pain intensity.
- Progestins and progesterone-releasing IUDs: Thin the uterine lining and suppress endometrial growth.
- GnRH agonists and antagonists: Temporarily induce a menopause-like state to stop estrogen production.
- Danazol (rarely used): Lowers estrogen levels but can have side effects, so it’s prescribed selectively.

While hormonal therapy can relieve pain effectively, it may cause side effects such as mood changes, weight gain, or irregular bleeding. Regular follow-up with a specialist ensures that the benefits outweigh the risks.
Pain Relief and Anti-Inflammatory Medications
Pain management forms the foundation of early treatment. NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) like ibuprofen help reduce menstrual pain and inflammation. However, they don’t treat the underlying disease and are most effective when used alongside hormonal therapy.
For chronic pelvic pain, doctors may combine medication with physiotherapy, yoga, or relaxation exercises. Personalized endometriosis pain management programs at Mayflower Hospital also address lifestyle factors such as stress, sleep, and diet, which influence pain perception.
Natural and Lifestyle-Based Approaches
Many women explore endometriosis natural treatment methods to complement medical care. Dietary changes – such as reducing red meat, caffeine, and processed foods – may help lower inflammation. Gentle exercise, stress management, and adequate hydration can also support hormonal balance.
Some patients benefit from supportive therapies like acupuncture, mindfulness, or pelvic floor physiotherapy. These do not replace medical treatment but can enhance overall comfort and recovery when guided by qualified specialists.
Mayflower’s multidisciplinary team combines medical, nutritional, and psychological care to ensure each patient receives a holistic approach to healing.
Surgical Treatment for Endometriosis
When medical or hormonal therapies fail to control symptoms, or when fertility becomes a major concern, surgery is often the next step in comprehensive endometriosis care. Surgical intervention aims to remove endometrial lesions, restore normal anatomy, and significantly reduce pain. The most effective and widely accepted method today is laparoscopic surgery, which allows both diagnosis and treatment through a minimally invasive approach.
Endometriosis Laparoscopy – The Gold Standard
Endometriosis laparoscopy is considered the gold standard for both diagnosis and treatment. During the procedure, a small camera (laparoscope) is inserted through tiny abdominal incisions, allowing surgeons to identify and remove visible endometrial implants. This method ensures precision, minimal scarring, and quicker recovery compared to open surgery.
Laparoscopy can involve two main techniques:
- Ablation: Burns or vaporizes endometrial tissue using heat or laser.
- Excision: Surgically removes the tissue from its root, offering better long-term relief and reduced recurrence.

At Mayflower Women’s Hospital, our specialists perform advanced laparoscopic excision procedures designed to preserve fertility while reducing pain and recurrence.
Endometriosis Excision Surgery Recovery and Outcomes
Endometriosis excision surgery recovery varies from patient to patient, depending on the extent of the disease and the complexity of the operation. Most women resume normal activities within two to four weeks. Post-surgery, mild bloating, fatigue, or shoulder pain from gas used during laparoscopy are common but temporary.
To maintain long-term results, many doctors recommend continuing hormonal therapy after surgery to prevent new lesions from forming. Recovery also involves rest, balanced nutrition, and follow-up visits to monitor progress. Patients often experience significant pain reduction, improved menstrual regularity, and higher fertility success rates.
Risks and Complications of Endometriosis Surgery
While laparoscopy is a safe and effective procedure, all surgeries carry some risks. Common endometriosis surgery risks include infection, bleeding, or scar tissue formation (adhesions). In rare cases, deep lesions near organs like the bladder or bowel may require additional surgical expertise.
Choosing an experienced surgical team greatly minimizes these risks. At Mayflower, every surgery is performed under expert supervision using advanced imaging guidance to ensure safety and precision. The hospital’s minimally invasive techniques reduce post-operative pain and shorten hospital stays, helping women return to normal life faster.
Comparing Medication vs Surgery for Endometriosis
Choosing between medication and surgery for endometriosis depends on multiple factors – such as disease stage, symptom intensity, fertility goals, and overall health. Both approaches aim to reduce pain and improve quality of life, but their mechanisms, outcomes, and timelines differ significantly. Understanding these differences helps women and their doctors design a plan that offers the best long-term results.
Effectiveness Across Disease Stages
In early or mild endometriosis, medical management with hormonal therapy and anti-inflammatory medications can effectively suppress symptoms and slow progression. These treatments work best when lesions are minimal and fertility is not an immediate concern.
However, in moderate to severe cases – especially when cysts, adhesions, or organ involvement are present – laparoscopic surgery often delivers better outcomes. Surgical removal of lesions provides direct relief from the source of pain, restores pelvic anatomy, and can significantly improve fertility rates.
Doctors frequently recommend a combined approach: medication to control hormones before or after surgery, ensuring both symptom relief and long-term disease control.
Short-Term Relief vs Long-Term Results
Medical treatments are ideal for short-term symptom control and can delay the need for surgery. However, once medication is stopped, symptoms often return. In contrast, surgery – particularly excision – addresses the root cause by removing endometrial tissue from the affected areas.
While surgery offers longer-lasting results, it’s not a guaranteed cure, as endometriosis can recur. Combining post-surgical hormonal therapy and lifestyle management often yields the best balance between relief and recurrence prevention.
Recovery and Lifestyle Considerations
Recovery and side effects differ for each approach. Medical management can cause side effects such as mood swings, bloating, or irregular bleeding but requires no downtime. Surgery, on the other hand, demands a few weeks of recovery but generally leads to substantial, lasting relief from pain.
During endometriosis surgery recovery, most patients return to work within two to four weeks and notice improved energy and mobility soon after. Those managing their condition medically may continue working uninterrupted but need consistent monitoring to manage side effects.
Lifestyle and emotional well-being are key to success in both approaches. Exercise, stress reduction, and a supportive care environment significantly influence overall recovery and comfort.
Cost and Accessibility in India
In India, endometriosis treatment cost varies widely based on the chosen approach. Medical management is relatively affordable on a short-term basis but can become costly over time due to recurring medication expenses.
Laparoscopic surgery has a higher upfront cost but provides longer-lasting relief and reduces repeated medication needs. Many insurance plans cover surgical procedures, especially when medically indicated. At Mayflower Women’s Hospital, patients receive transparent cost breakdowns and individualized treatment planning to ensure the most value-driven and effective care.
Comparison Table: Medication vs Surgery for Endometriosis
| Aspect | Medication | Surgery |
|---|---|---|
| Goal | Symptom control | Lesion removal |
| Effectiveness | Good for mild cases | Best for moderate to severe |
| Duration | Temporary | Long-term relief |
| Recovery Time | None | 2–4 weeks |
| Side Effects | Hormonal changes, fatigue | Minimal post-op discomfort |
| Fertility Benefit | Limited | Significant improvement |
| Cost Outlook | Lower upfront, recurring expenses | Higher upfront, lasting results |
When to Consider Surgery Over Medication
While many women benefit from medical therapy, there are certain situations where surgery for endometriosis becomes the more effective and sometimes necessary option. Surgery is usually recommended when the condition severely affects quality of life, fertility, or when other treatments have failed to control symptoms. Knowing when to transition from medication to surgical care ensures timely relief and prevents further complications.
Persistent Pain Despite Medical Management
If pain remains severe even after months of hormonal therapy or painkillers, surgery is often the next logical step. In such cases, laparoscopic excision surgery directly targets and removes lesions responsible for inflammation and nerve irritation. Persistent pain despite medication may indicate deep infiltrating endometriosis, which can only be treated effectively through surgical removal.
Fertility Preservation and Pregnancy Goals
For women trying to conceive, surgery for endometriosis can play a critical role. Hormonal treatments often suppress ovulation, making pregnancy difficult during therapy. Surgical removal of cysts, adhesions, and scar tissue improves the chances of natural conception by restoring pelvic anatomy and function.
At Mayflower Women’s Hospital, fertility-preserving laparoscopic techniques are used to maximize ovarian health while carefully excising endometriotic lesions. The procedure often helps women achieve better outcomes with natural conception or assisted reproductive techniques like IVF.
Severe Lesions or Organ Involvement
When endometriosis affects organs such as the bladder, bowel, or ureters, conservative management is rarely enough. Surgery becomes essential to prevent organ damage, manage pain, and restore normal function. Surgeons at Mayflower use advanced imaging and precision techniques to safely treat deep lesions while minimizing surgical trauma.
Diagnostic Uncertainty or Cystic Growths
If imaging or clinical findings suggest ovarian cysts (endometriomas) or other pelvic abnormalities, laparoscopy serves both as a diagnostic and therapeutic procedure. It allows doctors to confirm the diagnosis, assess disease severity, and remove problematic cysts in a single minimally invasive session.
In all these cases, expert evaluation is key. Mayflower Women’s Hospital offers a multidisciplinary approach that combines diagnostic imaging, advanced laparoscopy, and hormonal therapy to ensure the most balanced and effective care for every patient.
Post-Treatment Care and Preventing Recurrence
Recovery after endometriosis treatment – whether through medication or surgery – doesn’t end once the symptoms subside. Long-term success depends on ongoing management, hormonal balance, and lifestyle adjustments. A well-planned post-treatment care routine helps prevent recurrence, supports fertility, and maintains overall well-being.

Regular Follow-Up and Monitoring
Endometriosis can recur in some women, even after successful treatment. Regular follow-up visits allow doctors to monitor pain patterns, menstrual cycles, and hormonal response. For patients who underwent surgery, these check-ups help detect any regrowth of lesions early.
Specialists often recommend periodic pelvic exams, imaging studies, and in some cases, maintenance hormonal therapy to keep estrogen levels stable. Early intervention during follow-ups can prevent minor symptoms from escalating into severe pain again.
Hormonal Balance and Maintenance Therapy
After surgery, short- or long-term hormonal therapy for endometriosis may be prescribed to minimize recurrence. These treatments suppress new lesion formation and regulate menstrual cycles. Options include oral contraceptives, progestin-only pills, or GnRH analogs in adjusted doses.
Patients who respond well to medical therapy might continue low-dose maintenance regimens under medical supervision. The goal is to prevent new tissue growth while ensuring minimal side effects and sustained comfort.
Nutrition, Lifestyle, and Stress Management
Lifestyle plays a significant role in long-term recovery. A nutrient-rich, anti-inflammatory diet – high in fruits, vegetables, and omega-3 fatty acids – can help manage inflammation and hormonal fluctuations. Regular physical activity improves blood flow, boosts mood, and reduces pelvic pain.
Mind-body therapies such as yoga, meditation, and pelvic floor exercises have shown positive results in improving quality of life. Emotional health is equally important; joining support groups or counseling can help women navigate the challenges of living with a chronic condition.
Preventing Recurrence through Integrated Care
At Mayflower Women’s Hospital, post-treatment programs are designed to promote long-term stability. Combining medical therapy, physiotherapy, and routine follow-ups ensures that every patient receives continuous care beyond the operating room. Our multidisciplinary approach focuses on pain relief, hormonal control, and fertility protection, helping women maintain symptom-free lives for years.
Choosing the Right Approach for You
Selecting the right approach to manage endometriosis is a highly personal decision. Every woman’s journey with the condition is unique – defined by the stage of the disease, symptom severity, lifestyle priorities, and fertility goals. Whether you’re considering ongoing medication or planning for surgery, it’s essential to make this choice with guidance from a qualified endometriosis specialist.
Personalized Treatment Planning
At Mayflower Women’s Hospital, treatment begins with a thorough evaluation that includes medical history, physical examination, and imaging tests such as pelvic MRI for endometriosis diagnosis. These assessments help determine whether your condition can be managed through medical therapy or if surgical intervention is necessary.
Personalized care ensures you don’t receive a “one-size-fits-all” plan. Mild or early-stage endometriosis may respond well to non-surgical treatments, while advanced or recurrent cases benefit more from laparoscopic excision surgery. The aim is always to maximize relief, minimize recurrence, and preserve fertility.
Importance of Specialist Consultation
Endometriosis requires expertise that goes beyond routine gynecologic care. Consulting an endometriosis specialist ensures you receive targeted evaluation and the most effective treatment strategies. Specialists at Mayflower combine medical, surgical, and fertility expertise to provide comprehensive solutions under one roof.
Their holistic approach integrates hormonal therapy, surgical precision, nutritional counseling, and emotional support – ensuring each patient receives care aligned with both medical needs and life goals.
Why Choose Mayflower Women’s Hospital
As a leading center for women’s health in Ahmedabad, Mayflower Women’s Hospital offers advanced diagnostic tools, minimally invasive laparoscopy, and post-treatment rehabilitation under one integrated care model. The hospital’s dedicated team of gynecologists, radiologists, and physiotherapists work collaboratively to deliver evidence-based, patient-centered care.
From accurate diagnosis to compassionate recovery support, every step of the journey is designed for lasting well-being. Whether you’re exploring endometriosis medication vs surgery, seeking fertility preservation, or managing recurrent symptoms, Mayflower’s specialists provide the clarity and confidence needed to choose the right path.
If you’re struggling with chronic pelvic pain or suspect endometriosis, schedule a consultation with our expert gynecologists at Mayflower Women’s Hospital today. Discover your best treatment plan and take the first step toward a pain-free, empowered life.
Conclusion
Choosing between medication and surgery for endometriosis is not about finding a single “best” solution. It’s about identifying the right treatment at the right time for your body, symptoms, and long-term goals. As this comparison shows, endometriosis treatment options range from non-surgical medical management that controls symptoms to advanced laparoscopic surgery that directly removes disease-causing lesions. Each approach has a clear role depending on disease stage, pain severity, fertility plans, and response to previous treatments.
For women with mild symptoms, hormonal therapy and pain management can provide meaningful relief and help maintain daily functioning. However, when pain persists, fertility is affected, or the disease progresses, laparoscopic excision surgery often offers longer-lasting improvement and better quality of life. Importantly, combining surgery with appropriate post-treatment medical care can significantly reduce the risk of recurrence.
At Mayflower Women’s Hospital, endometriosis care is never one-dimensional. From accurate diagnosis using advanced imaging to personalized treatment planning and long-term follow-up, every step is designed around patient safety, comfort, and outcomes. With a multidisciplinary team and expertise in both medical and surgical management, Mayflower ensures that women receive clear guidance and evidence-based care at every stage of their journey.
If you’re living with chronic pelvic pain or suspect endometriosis, early evaluation can make a meaningful difference. Understanding your options today is the first step toward lasting relief, restored confidence, and improved well-being.
FAQs
Currently, there is no absolute cure for endometriosis, but the condition can be effectively managed through the right combination of medical and surgical treatments. Laparoscopic excision surgery offers long-term relief by removing visible lesions, while ongoing hormonal therapy helps prevent recurrence. With proper management and follow-up care, many women live symptom-free for years.
No. Surgery is not always necessary. Mild or early-stage endometriosis often responds well to non-surgical treatment like hormonal therapy and pain management. However, if symptoms persist or fertility is affected, surgery becomes the preferred approach. A specialist evaluation helps determine when surgical intervention is the most beneficial option.
Endometriosis surgery recovery typically ranges from two to four weeks, depending on the extent of the procedure. Patients usually experience reduced pelvic pain and improved mobility within days after laparoscopic surgery. Gentle activity, hydration, and follow-up appointments support faster healing and long-term comfort.
The most effective non-surgical treatments for endometriosis include hormonal therapy (oral contraceptives, progestins, or GnRH agonists), anti-inflammatory medications for pain, and lifestyle modifications such as diet and exercise. These therapies work best for managing mild cases or maintaining results after surgery.
In some cases, endometriosis recurrence may occur even after successful treatment. The risk is higher if lesions are deep or widespread. However, regular follow-ups, hormonal therapy, and lifestyle management greatly reduce recurrence chances. At Mayflower Women’s Hospital, patients receive structured post-treatment care to help sustain long-term results.
Author
-

Dr. Smeet, true to his name, is known for his warm personality and cheerful smile that make patients instantly feel at ease with him.
Until now, he has performed 8000+ surgeries and several of which are supra-major surgeries for deep infiltrating endometriosis and fertility enhancing surgeries. With several publications in notable journals, he is constantly pushing the envelope of possibilities in gynecological surgeries