Cervical cancer screening guidelines play a vital role in helping women over 30 protect their long-term reproductive health. Regular screening detects precancerous or abnormal cell changes in the cervix before they turn into cancer – giving women the power of prevention through early action.
After the age of 30, cervical health requires consistent attention. While cervical cancer remains one of the most preventable cancers in women, it continues to be one of the most common globally – especially in developing regions like India. The introduction of regular Pap smear and HPV test screening has drastically reduced incidence and mortality rates, making early testing one of the strongest defenses available today.
Understanding the right time, frequency, and method of screening helps ensure you’re neither under-tested nor over-tested. For women in their 30s and beyond, these cervical cancer screening guidelines serve as a roadmap – explaining when to test, which test to choose, and when to consult your gynecologist.
P (Bridge): In this guide, we’ll explore the importance of regular cervical screening, differences between Pap smear and HPV testing, recommended frequencies, and how hospitals like Mayflower Women’s Hospital provide complete preventive care for women’s health.
Why Cervical Cancer Screening Matters After 30
Once women cross the age of 30, cervical cancer screening becomes an essential part of preventive health care. During these years, hormonal changes, lifestyle factors, and long-term exposure to certain infections – particularly Human Papillomavirus (HPV) – can increase the risk of cervical cell abnormalities. Regular screening ensures that any early cellular changes are identified and treated before they progress to cancer.
According to the World Health Organization (WHO), cervical cancer is the fourth most common cancer among women globally, yet it is largely preventable through routine screening and timely treatment. Studies show that women who undergo Pap smears or HPV tests at recommended intervals are far less likely to develop advanced disease. This is because these tests can detect subtle changes in cervical cells years before any symptoms appear.
In India, where awareness about cervical screening after 30 is still growing, consistent testing can make a life-saving difference. Many women delay or skip screenings due to misconceptions, discomfort, or lack of information. However, medical experts emphasize that a simple Pap test takes just a few minutes and can significantly reduce the risk of developing cervical cancer.
Whether you’re planning a family, approaching menopause, or simply prioritizing your wellness, understanding why cervical screening matters is the first step toward empowerment. Next, let’s explore how cervical cancer develops and which risk factors you should be aware of.
Understanding Cervical Cancer and Its Risk Factors
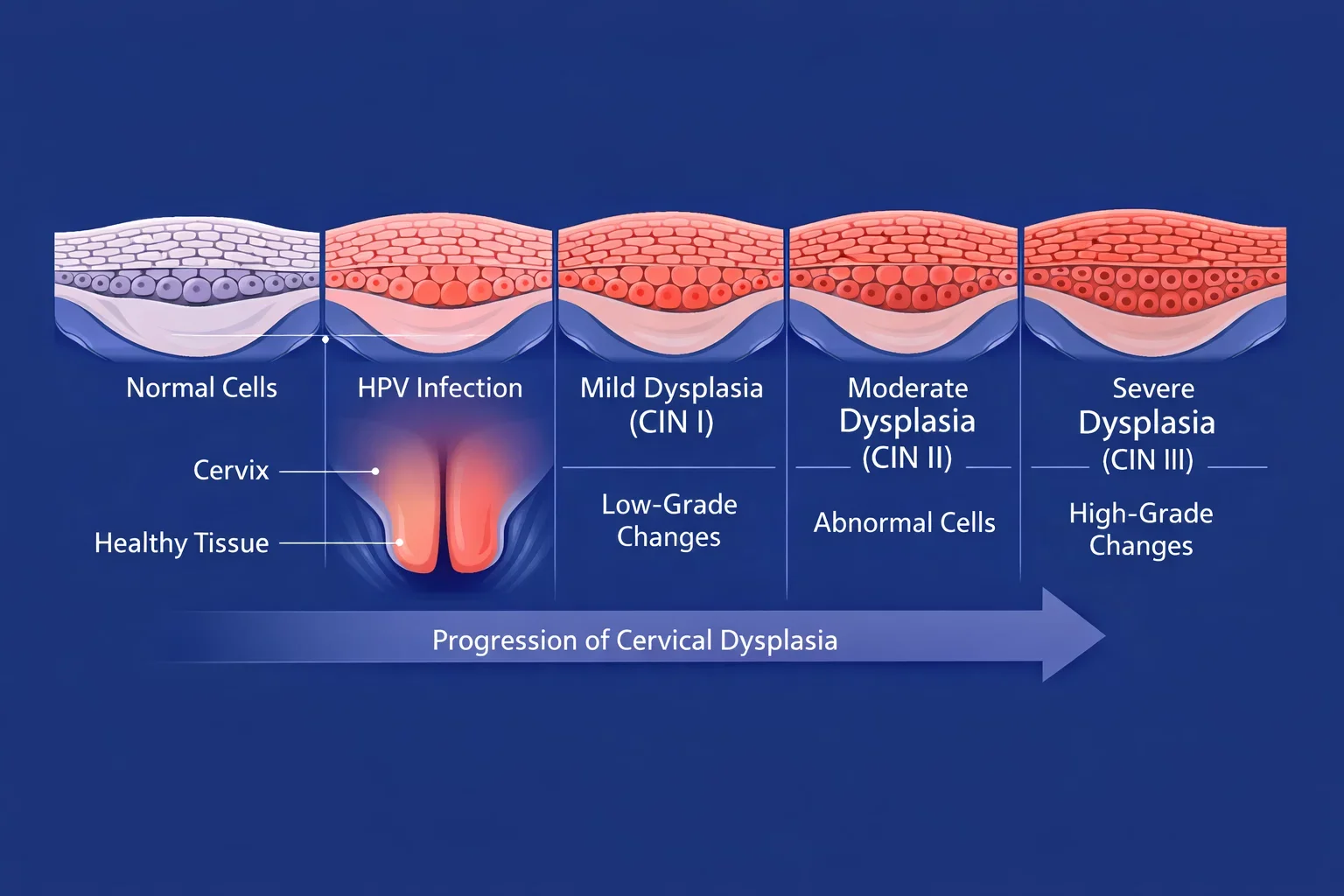
Cervical cancer begins in the cells lining the cervix – the lower part of the uterus that connects to the vagina. It develops gradually when normal cells undergo changes (called dysplasia) and, if left untreated, can become cancerous over time. Fortunately, this process takes several years, giving regular cervical cancer screening an opportunity to catch abnormalities early and prevent cancer before it starts.
The Human Papillomavirus (HPV) is the primary cause of cervical cancer. It’s a common sexually transmitted infection, and most sexually active women will encounter at least one strain during their lifetime. While many HPV infections resolve naturally, certain high-risk strains – notably HPV types 16 and 18 – can persist and cause cellular changes in the cervix. That’s why HPV test guidelines emphasize screening for these specific strains in women aged 30 and above.
Beyond HPV, several other risk factors can increase a woman’s chances of developing cervical cancer. These include early onset of sexual activity, having multiple sexual partners, smoking, weakened immunity (such as HIV infection), long-term use of oral contraceptives, and poor genital hygiene. Family history of cervical or other gynecologic cancers can also elevate risk.
Understanding these risk factors helps women take preventive steps – from vaccination and safe sexual practices to timely screening. A Pap smear or HPV test can detect even minor cellular abnormalities, offering peace of mind and early intervention.
Recognizing the underlying risks is important, but being aware of the early warning signs and symptoms can help women seek medical advice sooner. Let’s explore how to identify these changes and when to consult your gynecologist.
Early Symptoms and Warning Signs to Watch
One of the challenges of cervical cancer is that it often shows no symptoms in its early stages. This makes regular cervical cancer screening crucial, as tests like the Pap smear and HPV test can detect abnormal changes in the cervix long before symptoms develop. However, being aware of potential warning signs ensures that women can act quickly if something feels unusual.
The most common early symptom is abnormal vaginal bleeding, which may occur between menstrual periods, after sexual intercourse, or post-menopause. Some women notice unusual vaginal discharge – watery, blood-stained, or foul-smelling. Persistent pelvic pain, pain during intercourse, or a general sense of discomfort in the lower abdomen can also signal that something isn’t right.
These symptoms don’t always mean cancer, but they should never be ignored. In many cases, infections or benign conditions can cause similar signs – which is why consultation with a gynecologist and appropriate cervical screening after 30 are essential to determine the cause accurately.
Women who have missed regular screenings or have known risk factors like HPV infection, smoking, or family history should be especially alert to these symptoms. Early medical evaluation not only ensures timely diagnosis but also enables simpler, less invasive treatment if required.
Now that we understand the symptoms and risk factors, let’s move into the core of this article – the official cervical cancer screening guidelines that outline how and when women above 30 should get tested.
Cervical Cancer Screening Guidelines Explained
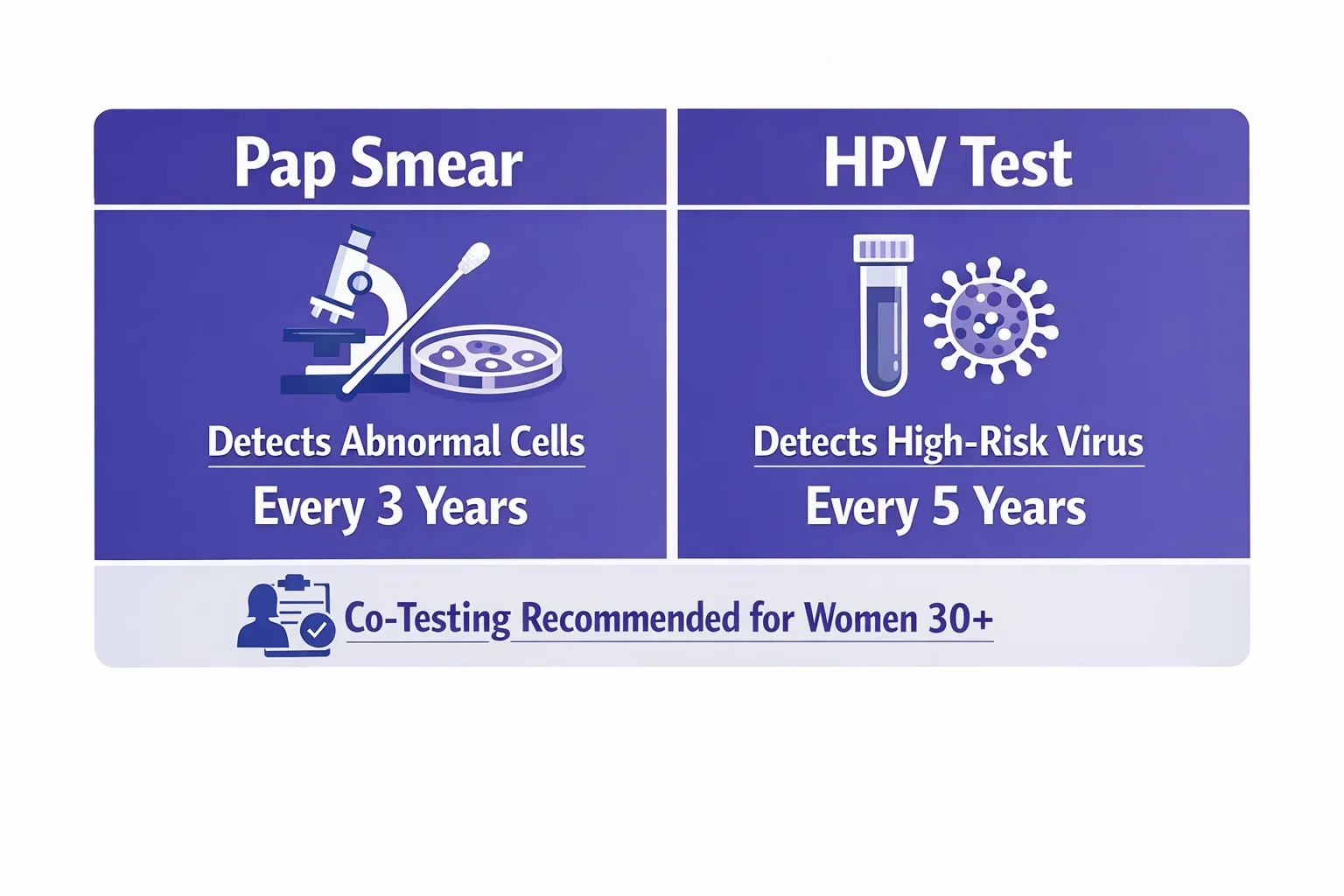
Regular cervical cancer screening is the most effective way to prevent the disease. For women aged 30 and above, both Pap smears and HPV tests are recognized as reliable methods to detect abnormal cervical cell changes or HPV infections early. Let’s explore what each test involves, how often they should be done, and why co-testing is often the most comprehensive approach.
Pap Smear Guidelines for Women 30+
The Pap smear test (also called a Pap test) is a simple, quick, and highly effective method used to examine cells from the cervix. During the test, your gynecologist gently collects a small sample of cells from the cervical surface using a soft brush or spatula. These cells are then analyzed under a microscope to identify any irregularities, infections, or pre-cancerous changes.
For women over 30, Pap smear guidelines recommend screening once every three years if the results are normal. If abnormalities are found, your doctor may suggest repeating the test sooner or performing additional diagnostic tests, such as colposcopy or HPV DNA testing, for closer evaluation.
Factors like previous abnormal results, weakened immunity, or HIV infection may require more frequent Pap smears. Women who have undergone a hysterectomy for non-cancerous reasons and have no history of cervical abnormalities may not need further Pap testing – though this should always be confirmed with a gynecologist.
While Pap smears are crucial for detecting abnormal cells, they don’t directly test for HPV, which is why the HPV test plays an equally vital role in cervical cancer prevention.
HPV Test Guidelines for Women 30+
The HPV test screens specifically for the presence of high-risk HPV strains – mainly HPV 16 and 18 – that can cause cervical cell changes. It involves collecting a sample in the same way as a Pap test but uses molecular techniques to detect viral DNA instead of examining cells under a microscope.
According to international and Indian cervical screening recommendations, women aged 30–65 years should get an HPV test every five years if results are normal. When combined with a Pap smear, this interval remains the same but provides a stronger layer of protection through co-testing.
The HPV test is especially helpful for women who’ve had inconclusive Pap results or a previous history of HPV infection. It helps identify persistent infections early – long before visible abnormalities develop – allowing your doctor to monitor and manage your risk effectively.
Both tests serve unique but complementary purposes. For most women over 30, combining the two offers the most accurate protection.
Co-Testing – The Best of Both Worlds
Co-testing combines the Pap smear and HPV test in one screening session. This dual approach enhances accuracy by detecting both cellular changes and the underlying viral cause. Most experts, including the World Health Organization (WHO) and American Cancer Society (ACS), recommend co-testing every five years for women aged 30–65.
Co-testing reduces the chances of false negatives and provides longer reassurance between tests. If both results are negative, the likelihood of developing cervical cancer within the next few years is extremely low. However, if either test shows abnormal results, your doctor will recommend further investigation or closer follow-up.
Women should note that screening isn’t a one-size-fits-all recommendation. Your medical history, family background, and personal risk factors all play a part in determining how often you should test. A discussion with your gynecologist ensures you receive a personalized plan that aligns with your health profile.
Understanding these official cervical cancer screening guidelines helps women make confident, informed choices. But how often should you actually get tested, and when can screening stop? Let’s address those next.
How Often Should You Get a Pap Smear or HPV Test?
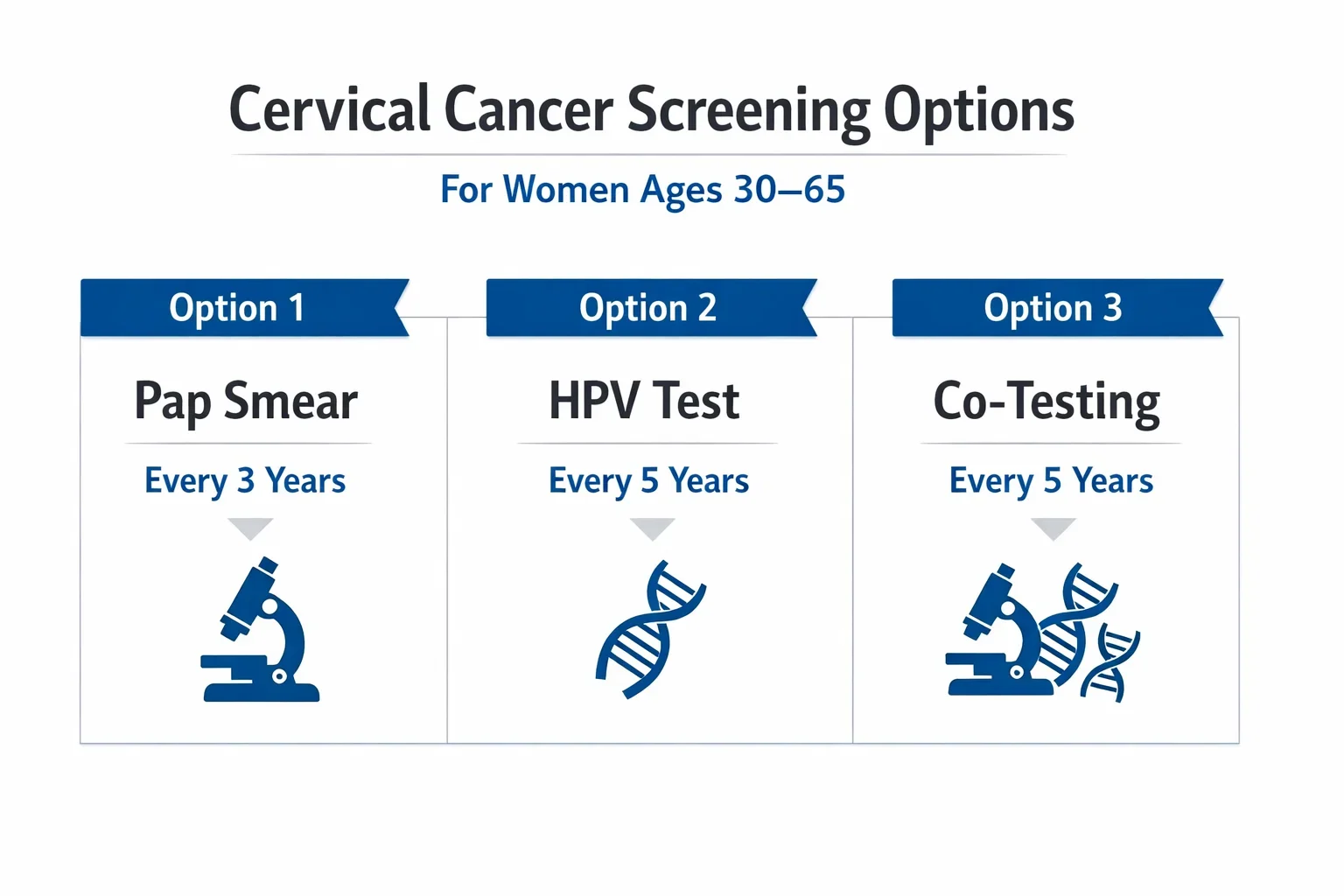
One of the most common questions women ask is, “How often should I get a Pap smear?” The answer depends on your age, health history, and past test results. For women between 30 and 65 years, both global and Indian cervical screening guidelines recommend one of three safe options:
- Pap smear every 3 years if results remain normal.
- HPV test every 5 years if results are negative.
- Co-testing (Pap + HPV) every 5 years for maximum reassurance.
These intervals are based on years of research showing that cervical cancer develops slowly. If both tests are normal, repeating them too frequently offers little additional benefit. However, women with abnormal Pap results, persistent HPV infection, weakened immunity, or a previous diagnosis of pre-cancerous lesions may need earlier or more frequent testing as advised by their gynecologist.
For women over 65, most experts recommend that cervical screening can safely stop if they’ve had at least three consecutive normal Pap results or two negative HPV tests in the past 10 years, with no abnormal findings in the last 5 years. Screening may also stop after a total hysterectomy performed for non-cancerous reasons, provided there is no history of cervical cell changes.
If you ever experience symptoms such as abnormal bleeding, pelvic pain, or unusual discharge, you should not wait for your next scheduled screening – book an evaluation immediately. Early consultation ensures that any new concerns are addressed without delay.
Understanding frequency is important, but many women still wonder which test they should choose. Let’s compare the Pap smear vs HPV test to help you decide what’s best for you.
Pap Smear vs HPV Test – Which Is Right for You?
Both the Pap smear and HPV test are vital tools in detecting early changes that can lead to cervical cancer. Yet, many women over 30 are unsure which one they should choose or whether both are necessary. Understanding how these tests differ helps you make an informed decision that best suits your health profile and comfort.
The Pap smear focuses on examining cervical cells under a microscope to look for abnormalities. The HPV test, on the other hand, checks for the presence of the high-risk virus strains (mainly HPV types 16 and 18) that can cause those abnormalities. While both serve the same preventive purpose, their mechanisms and frequency recommendations vary slightly.
Comparison Table: Pap Smear vs HPV Test
| Feature | Pap Smear | HPV Test |
|---|---|---|
| Purpose | Detects abnormal cervical cells | Detects high-risk HPV infection |
| Recommended Frequency (Age 30–65) | Every 3 years (if normal) | Every 5 years (if negative) |
| Method | Microscopic cell examination | Molecular testing for HPV DNA |
| Result Timeline | Usually 1–2 weeks | 1–2 weeks |
| Accuracy for Detecting HPV-Linked Risk | Moderate | High |
| Can Be Combined (Co-testing) | Yes, every 5 years | Yes, every 5 years |
| Best For | Detecting existing cell changes | Identifying underlying infection early |
If you’ve had a history of abnormal Pap results, combining both tests through co-testing offers a more comprehensive view of your cervical health. This approach is particularly recommended for women above 30, as it minimizes the risk of missed detection and provides longer intervals between screenings when results are clear.
The Pap smear vs HPV test debate is not about choosing one over the other – it’s about understanding how both complement each other. Pap tests detect changes already occurring, while HPV tests identify risks before changes happen. When used together, they provide the highest level of safety and confidence.
Once you’ve chosen your screening method, it’s equally important to know about cost and access. Let’s explore how affordable and accessible cervical screening is across India and why choosing a trusted healthcare provider like Mayflower Women’s Hospital makes all the difference.
Cost and Accessibility of Cervical Screening in India
One of the best things about modern cervical cancer screening is that it’s both affordable and widely available. The Pap smear test cost in India generally ranges between ₹600 and ₹1,500, depending on the hospital, city, and whether it’s part of a preventive health package. When combined with an HPV test, the cost may rise to ₹2,000–₹3,500 – but this dual approach offers a more accurate and longer-lasting safeguard.
Many healthcare providers, including Mayflower Women’s Hospital, offer comprehensive women’s health checkup packages that include Pap smear and HPV testing at a bundled rate. These packages not only make preventive screening cost-effective but also ensure that testing is performed under hygienic conditions by qualified specialists, ensuring comfort, accuracy, and privacy.
Accessibility has also improved significantly. Cervical screening is now offered in most urban hospitals, diagnostic centres, and gynaecology clinics across India. With increasing awareness, more women are choosing to undergo regular tests as part of their annual health checkups – a small investment that can prevent major health complications in the future.
While price is an important factor, the quality of care and expertise of the medical team matter even more. At Mayflower Hospital, every screening is supervised by experienced gynecologists using advanced diagnostic technology, ensuring the most reliable results and compassionate patient care.
Understanding the costs is helpful, but knowing when to consult a doctor is equally vital. In the next section, we’ll look at the signs that indicate you should speak to your gynecologist sooner rather than later.
When to Consult a Gynecologist
Even with normal screening results, it’s important to stay alert to any new or unusual symptoms. You should consult a gynecologist immediately if you experience abnormal bleeding, persistent pelvic pain, unusual discharge, or discomfort during intercourse. These signs don’t always indicate cancer, but they can point to infections or cellular changes that need timely attention.
Women with a family history of cervical cancer, HPV infection, or a history of abnormal Pap smear results should be especially proactive about follow-up appointments. Your doctor might recommend repeat testing or closer observation to ensure your cervix remains healthy.
If you’ve had a hysterectomy or have entered menopause, your doctor will guide you on whether to continue or stop screening based on your personal medical history. Regular communication and annual gynecologic visits ensure early detection of any emerging issues.
At Mayflower Women’s Hospital, our gynecologists provide patient-centric, evidence-based care – offering comfort, confidentiality, and clarity at every step. From counseling and screening to treatment, our specialists help women make informed choices about their reproductive health.
For women seeking a trusted environment to prioritize their well-being, Mayflower Hospital’s Preventive Care Unit ensures personalized cervical screening and comprehensive women’s health support.
Preventive Care at Mayflower Hospital
At Mayflower Women’s Hospital, preventive care is more than just routine testing – it’s a commitment to safeguarding every woman’s lifelong health. Our approach to cervical cancer screening combines advanced diagnostic technology with compassionate care, ensuring comfort, privacy, and confidence for women at every stage of life.

We provide both Pap smear and HPV testing under one roof, guided by international and Indian screening standards. Each test is performed by experienced gynecologists and laboratory experts who ensure accuracy and gentle handling throughout the process. For women above 30, our integrated Women’s Health Checkup Packages include all essential preventive screenings – making it easier to stay proactive about cervical and overall reproductive health.
What makes Mayflower’s preventive care unique is our patient-first approach. From pre-screening counseling to follow-up consultations, our medical team supports every woman through clear explanations, prompt results, and evidence-based advice. Whether you are screening for the first time or maintaining regular checkups, you’ll experience attentive, confidential care in a modern and comfortable environment.
Take a proactive step toward long-term wellness – book your cervical cancer screening at Mayflower Women’s Hospital today and protect your health with expert-led preventive care.
Conclusion
Regular cervical cancer screening is one of the most effective ways for women to protect their long-term health. By following the recommended Pap smear and HPV test schedules after the age of 30, women can detect and prevent potential issues long before they become serious. Early detection doesn’t just save lives – it preserves fertility, wellness, and peace of mind.
As medical science advances, screening has become faster, more accurate, and more comfortable. Whether you’re scheduling your first test or continuing routine checkups, staying consistent is key. Discuss your individual screening plan with your gynecologist to ensure it aligns with your medical history and lifestyle.
At Mayflower Women’s Hospital, our focus is on empowering women through preventive care. From accurate diagnostics to compassionate consultations, every service is designed to make healthcare approachable and trustworthy.
Take control of your health – book your cervical cancer screening at Mayflower Women’s Hospital today and stay one step ahead with expert-led preventive care.
FAQs
Women aged 30–65 should have a Pap smear every 3 years if results remain normal. If you combine it with an HPV test (co-testing), you can safely extend the interval to every 5 years. Your gynecologist may suggest more frequent tests if you’ve had abnormal results or additional risk factors.
A Pap smear may cause mild pressure or short-term discomfort, but it should not be painful. The procedure takes just a few minutes and is performed gently using sterile instruments. If you feel significant pain, inform your doctor so they can adjust the technique for comfort.
The Pap smear checks cervical cells for early abnormal changes, while the HPV test looks for the virus that causes those changes. For women 30+, both tests together offer the best protection by identifying risk early and confirming cervical cell health.
Most women can stop screening after 65 if they’ve had three consecutive normal Pap results or two negative HPV tests in the last 10 years, with no abnormal findings. Women who’ve had a hysterectomy for non-cancerous reasons may also stop, but this should always be confirmed with a gynecologist.
The Pap smear test cost usually ranges from ₹600 to ₹1,500, while HPV testing may cost between ₹2,000 and ₹3,500. Many hospitals, including Mayflower Women’s Hospital, offer these tests within affordable women’s health screening packages.
Author
-

Dr. Smeet, true to his name, is known for his warm personality and cheerful smile that make patients instantly feel at ease with him.
Until now, he has performed 8000+ surgeries and several of which are supra-major surgeries for deep infiltrating endometriosis and fertility enhancing surgeries. With several publications in notable journals, he is constantly pushing the envelope of possibilities in gynecological surgeries