Endometriosis and fertility are closely connected, affecting millions of women worldwide who dream of becoming mothers. Endometriosis occurs when tissue similar to the lining of the uterus grows outside the womb, often on the ovaries, fallopian tubes, or pelvic lining. This misplaced tissue reacts to hormonal changes each month, leading to inflammation, scarring, and sometimes severe pelvic pain.
For many women, the first sign of endometriosis is not just discomfort but difficulty in conceiving. The condition can interfere with ovulation, egg quality, or embryo implantation-all critical steps in achieving pregnancy. Yet, it’s important to remember that endometriosis does not automatically mean infertility. Many women with this condition successfully conceive, both naturally and with medical support.
Understanding the link between endometriosis and reproductive health empowers women to make informed choices. With today’s advances in diagnostic imaging, fertility treatments, and surgical care, managing endometriosis and achieving pregnancy has become more achievable than ever before.
Understanding Endometriosis and How It Affects the Reproductive System
What Is Endometriosis?
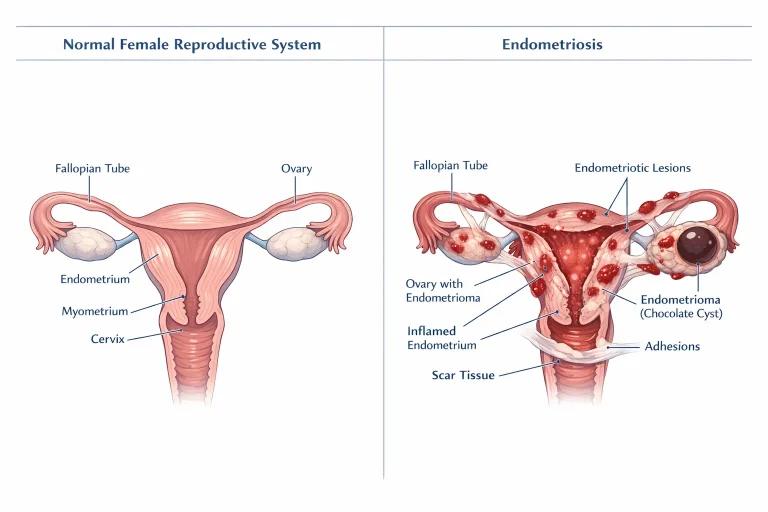
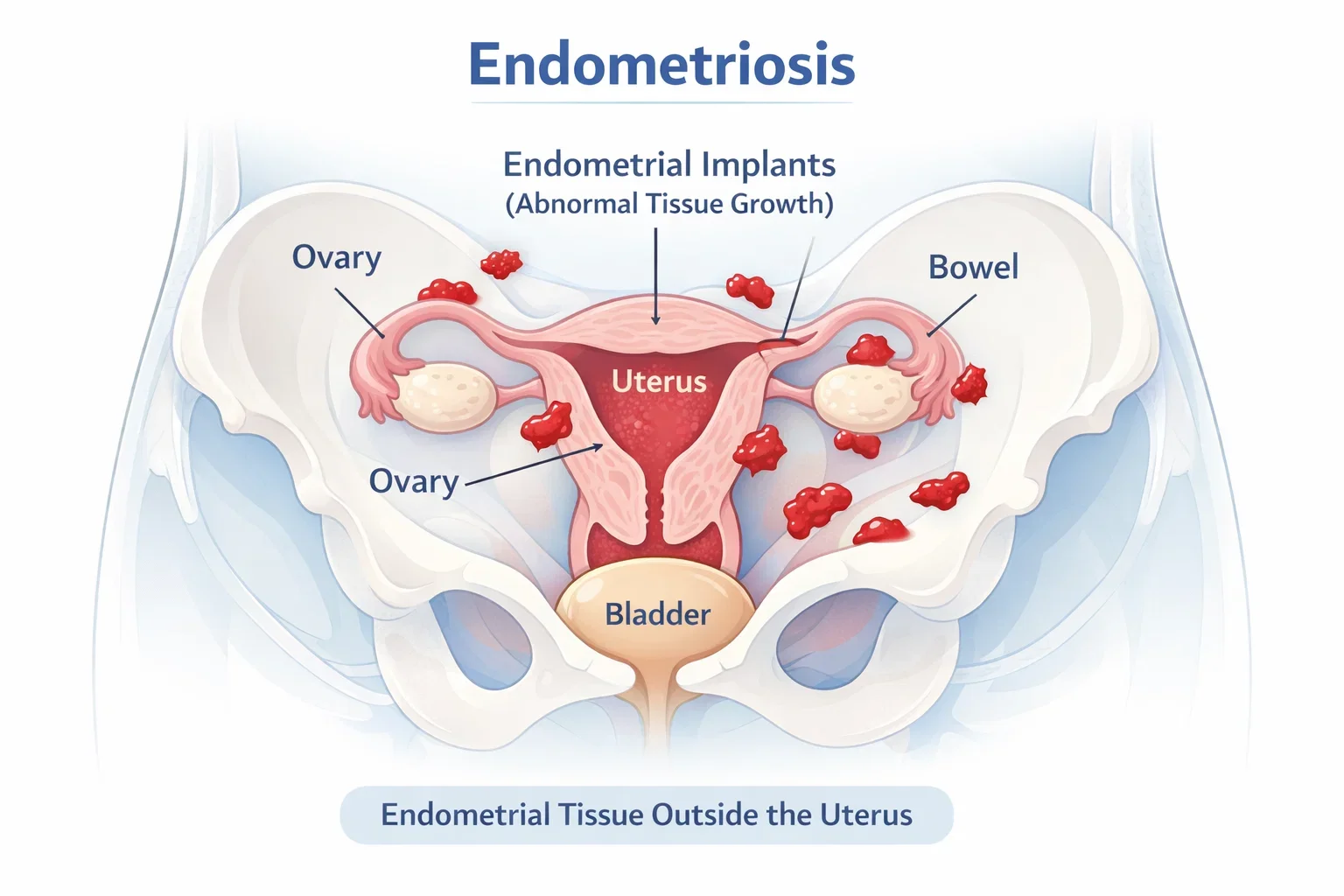
Endometriosis is a chronic condition where tissue similar to the inner lining of the uterus, known as the endometrium, begins to grow in areas where it doesn’t belong. These abnormal growths are often found on the ovaries, fallopian tubes, outer surface of the uterus, or other pelvic organs. Each month, this tissue responds to hormonal changes just like the uterine lining – it thickens, breaks down, and bleeds. However, unlike normal menstrual blood that leaves the body, this trapped tissue causes irritation, inflammation, and sometimes the formation of scar tissue or cysts.
The severity of symptoms varies widely. Some women experience debilitating menstrual cramps, pelvic pain, or pain during intercourse, while others may not realize they have the condition until they face challenges conceiving. Because of this, endometriosis is often underdiagnosed or mistaken for other gynecological issues, making awareness and early detection essential.
How Endometriosis Can Impact Fertility
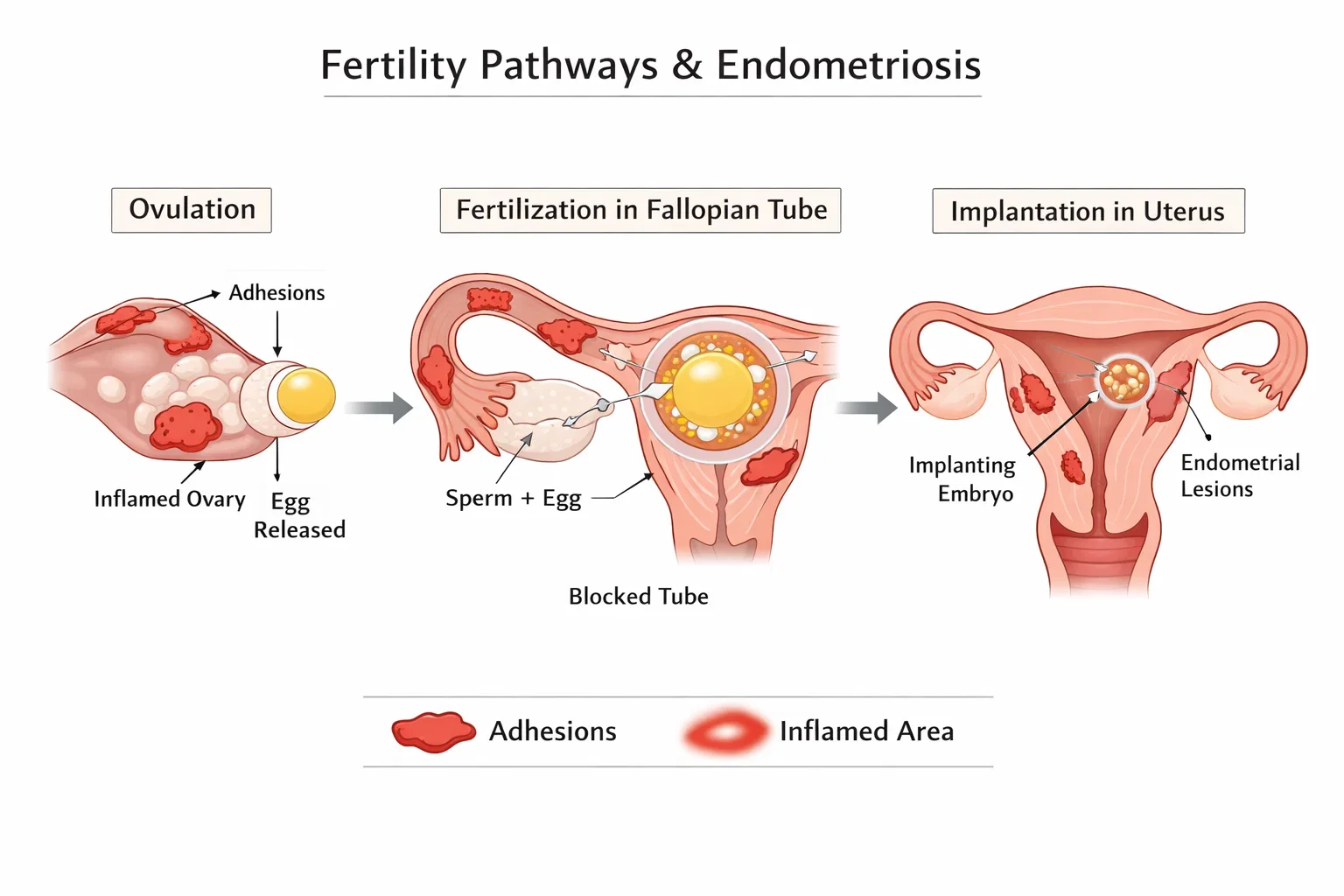
Endometriosis can affect fertility in several ways, depending on the extent and location of the lesions. In some women, the condition can distort the normal structure of the reproductive organs. Adhesions – bands of scar tissue that form as a result of inflammation – may block the fallopian tubes, preventing the egg and sperm from meeting. Ovarian cysts caused by endometriosis, called endometriomas, can also interfere with ovulation and reduce the quality of eggs.
Even in cases where the reproductive anatomy appears normal, microscopic inflammation can alter the environment within the pelvis, making it harder for embryos to implant successfully. The hormonal imbalance caused by endometriosis may further reduce fertility potential by affecting the release of eggs or the health of the uterine lining.
However, not every woman with endometriosis experiences infertility. Many conceive naturally, especially when the condition is diagnosed early and managed properly. Treatment plans that focus on reducing inflammation, preserving ovarian health, and maintaining reproductive function can make a meaningful difference in fertility outcomes.
Understanding how endometriosis affects the reproductive system helps women take the next step-exploring whether pregnancy is still possible. While the condition can create challenges, modern fertility care has transformed what used to be barriers into manageable paths toward motherhood.
Can You Get Pregnant with Endometriosis?
Levels of Endometriosis and Their Impact on Conception
The likelihood of becoming pregnant with endometriosis depends largely on how advanced the condition is and how it affects the reproductive organs. Doctors classify endometriosis into four stages – minimal, mild, moderate, and severe – based on the extent, location, and depth of endometrial growth.
In minimal and mild cases, endometrial tissue growth is limited and typically does not interfere with the function of the fallopian tubes or ovaries. Many women in these stages are able to conceive naturally with proper lifestyle care and medical monitoring. In moderate to severe cases, however, scar tissue, adhesions, and ovarian cysts may distort pelvic anatomy, making conception more difficult. These cases often require medical or surgical treatment to restore fertility potential.
While severity plays a role, it is not the only factor. Hormonal balance, egg quality, age, and general health also influence a woman’s ability to conceive. Some women with severe endometriosis get pregnant naturally, while others with mild disease may face more challenges. This is why personalized evaluation and care are essential for each individual.
Natural Conception with Endometriosis – Is It Possible?
Yes, it is possible to conceive naturally with endometriosis, especially when the condition is mild and managed proactively. Regular ovulation, open fallopian tubes, and a healthy uterine lining create a favorable environment for conception. Early detection and symptom management can help preserve these natural functions.
For women planning pregnancy, tracking ovulation and seeking timely fertility assessments can improve the chances of success. Lifestyle modifications – such as maintaining a balanced diet, reducing stress, and managing pain effectively – also play a key role.
However, if conception does not occur after several months of trying, consulting a fertility specialist is recommended. With the right guidance, many women with endometriosis go on to achieve healthy pregnancies, whether naturally or with the support of assisted reproductive treatments.
While medical and surgical treatments play a major role in improving fertility, long-term success also depends on the body’s overall balance. Adopting lifestyle and nutrition strategies can further support reproductive health and complement clinical care-especially for women planning pregnancy after endometriosis treatment.
Endometriosis Fertility Treatments Explained
Medical Treatments to Improve Fertility
When endometriosis interferes with the ability to conceive, several medical options can help restore balance and support reproductive health. Doctors often begin with medications designed to control hormonal fluctuations that drive the growth of endometrial tissue. These may include hormonal contraceptives, gonadotropin-releasing hormone (GnRH) agonists, or progestin-based therapies.
While these treatments do not cure endometriosis, they can reduce pain, suppress abnormal tissue growth, and improve ovulation regularity in some women. For those actively trying to conceive, medications such as ovulation-inducing agents can be prescribed under medical supervision to enhance the likelihood of natural conception. Each plan is customized according to the stage of endometriosis, age, and ovarian reserve, ensuring that fertility potential is optimized safely.
Surgical Treatment Options
When endometriosis has caused structural damage to the reproductive organs, surgery may be recommended to remove endometrial lesions, cysts, or scar tissue. Laparoscopic surgery is the most common and effective method used for this purpose. It allows surgeons to precisely identify and remove abnormal tissue while preserving the uterus and ovaries.
For women seeking to conceive, conservative laparoscopic procedures are preferred, as they help restore the natural anatomy of the pelvis. This can significantly increase the chances of pregnancy, especially when combined with lifestyle or fertility-focused care afterward. Recovery time is usually short, and many patients experience not only relief from pain but also improved fertility outcomes.
Assisted Reproductive Techniques (IVF, IUI, and More)
If natural conception or surgery alone does not result in pregnancy, assisted reproductive technologies (ART) offer promising alternatives. Intrauterine insemination (IUI) may be considered in mild to moderate cases of endometriosis, particularly when the fallopian tubes are open and sperm quality is healthy.
For more advanced stages, in vitro fertilization (IVF) is often the most effective approach. During IVF, eggs are retrieved from the ovaries, fertilized in a laboratory, and then transferred to the uterus. Studies show that IVF success rates in women with endometriosis are encouraging, especially when the condition is well-managed prior to treatment. Early consultation with an experienced fertility team can make a major difference in outcomes, allowing women to approach pregnancy with confidence and support.

Managing Endometriosis to Improve Fertility Naturally
Lifestyle Modifications That Support Fertility
Managing endometriosis isn’t only about medical treatments – it’s also about creating a healthy internal environment that supports reproductive function. Lifestyle adjustments play a vital role in reducing inflammation, balancing hormones, and improving overall well-being.
Regular physical activity helps improve blood circulation in the pelvic area and reduces stress hormones, both of which are beneficial for fertility. Gentle exercises like yoga, walking, and stretching can also relieve pain and tension. Adequate sleep and stress management are equally important, as chronic stress can disrupt hormonal balance and ovulation cycles.
Avoiding smoking and excessive alcohol intake, maintaining a healthy body weight, and keeping a consistent daily routine further contribute to better hormonal health. When these small yet consistent changes are combined with medical care, many women notice significant improvements in both symptom control and reproductive outcomes.
The Role of Nutrition – Endometriosis Fertility Diet
Nutrition plays a powerful role in managing endometriosis and enhancing fertility. A balanced endometriosis fertility diet focuses on reducing inflammation and supporting hormone balance. This typically includes foods rich in omega-3 fatty acids (like salmon and flaxseeds), antioxidants (such as berries and leafy greens), and plant-based proteins.
Avoiding processed foods, refined sugar, and excessive caffeine can also help minimize hormonal disruptions. Including plenty of fiber through vegetables, fruits, and whole grains assists in maintaining digestive health and regulating estrogen levels. Women are encouraged to consult a nutritionist to tailor their diet based on their body’s unique needs and fertility goals.
Emotional and Mental Well-being
Living with endometriosis can be emotionally exhausting, especially for women navigating fertility challenges. Anxiety, frustration, and uncertainty are common, but emotional support is just as crucial as physical care. Practicing mindfulness, joining support groups, or seeking counseling can help manage these feelings and promote a positive outlook.
Many women find strength in connecting with others who share similar experiences. This emotional stability not only improves mental health but can also positively influence hormonal balance and reproductive success. A holistic approach – where mental, physical, and reproductive health are aligned – provides the best foundation for achieving a healthy pregnancy.
Endometriosis and Pregnancy: What to Expect After Conception
Pregnancy with Endometriosis – Risks and Precautions
For many women, conceiving with endometriosis feels like a victory after years of uncertainty. However, pregnancy with endometriosis requires careful medical supervision to ensure both maternal and fetal well-being. While many women with endometriosis go on to have completely healthy pregnancies, some may face a slightly higher risk of complications such as preterm delivery, placenta previa, or cesarean birth due to scarring or inflammation in the pelvic region.
Regular prenatal checkups and early monitoring help identify and manage these risks effectively. Gynecologists often recommend individualized care plans that include frequent ultrasounds, nutritional monitoring, and specialized prenatal support. Pain management during pregnancy should also be carefully discussed, as certain medications may not be safe during this stage.
Maintaining a balanced diet, staying hydrated, managing stress, and following prescribed supplements – especially folic acid and iron – can help ensure a healthier pregnancy journey. Open communication with your healthcare team remains the most important aspect of safe and confident motherhood after endometriosis.
Endometriosis and Pregnancy Success Stories
Despite the challenges, countless women with endometriosis have achieved successful pregnancies, delivering healthy babies through natural conception or assisted treatments. These stories serve as a reminder that infertility is not a certainty – it’s a challenge that can be overcome with the right medical approach, persistence, and emotional resilience.
From women conceiving naturally after laparoscopic surgery to those finding success with IVF, each experience reinforces the importance of comprehensive care and early intervention. Sharing these journeys helps others facing similar struggles to stay hopeful and informed.

Mayflower Hospital continues to support women through every phase – from diagnosis and treatment to conception and delivery – ensuring that no woman feels alone in her fertility journey. The combination of medical expertise, compassionate care, and advanced reproductive technology makes healthy pregnancy outcomes possible for women living with endometriosis.
When to See a Fertility Specialist
Signs It’s Time for a Consultation
Knowing when to seek professional help is key for women with endometriosis who are planning to conceive. If you’ve been trying to get pregnant for six months or longer without success, it may be time to consult a fertility specialist – especially if you already have a diagnosis of endometriosis. Other signs that indicate a need for evaluation include severe pelvic pain during periods, pain during intercourse, or irregular menstrual cycles.
A fertility assessment can provide valuable insight into your ovarian reserve, hormone levels, and reproductive anatomy. Specialists can also identify other potential factors that might be affecting conception, such as fallopian tube blockages or hormonal imbalances. The earlier these issues are addressed, the better the chances of creating an effective, individualized treatment plan.
Even if you’re not actively trying to conceive, regular gynecological visits allow early detection and management of endometriosis, helping preserve fertility for the future. Early intervention remains one of the most effective tools for maintaining reproductive health and peace of mind.
Why Choose Mayflower for Endometriosis and Fertility Care
Choosing the right hospital for endometriosis and fertility treatment can make a significant difference in outcomes. At Mayflower Hospital, care is guided by evidence-based medicine and delivered by a multidisciplinary team of gynecologists, fertility specialists, and laparoscopic surgeons. Each patient receives personalized care – from accurate diagnosis through advanced imaging like MRI mapping, to fertility-focused interventions such as laparoscopy and assisted reproductive techniques.
The hospital’s integrated approach ensures that every aspect of reproductive health is addressed with precision and compassion. Patients benefit from access to modern fertility technologies, holistic recovery plans, and continuous emotional support throughout their journey. Whether you’re planning your first consultation or seeking advanced fertility solutions, Mayflower’s specialists are committed to helping you take confident steps toward motherhood.
Conclusion
Endometriosis and fertility are deeply connected, but a diagnosis does not define a woman’s ability to conceive. With the right care, early intervention, and ongoing support, many women with endometriosis successfully achieve pregnancy and experience healthy motherhood. Understanding your body, recognizing symptoms early, and seeking specialized care from a trusted team are the keys to positive outcomes.
At Mayflower Hospital, every woman’s fertility journey is treated with compassion, expertise, and personalized medical attention. From accurate diagnosis to advanced fertility treatments, the hospital’s multidisciplinary approach ensures that each patient receives comprehensive, evidence-based care designed to maximize reproductive health.
If you’re managing endometriosis and planning to conceive, take the first step by consulting with our fertility experts. Early guidance can make all the difference in preserving fertility, preventing complications, and building a healthy future.
Subscribe to our newsletter to read our article on Endometriosis and Pregnancy Success Stories-featuring inspiring journeys and medical insights from women who turned hope into reality.
FAQ: Endometriosis and Fertility
Yes. Endometriosis can cause infertility by affecting the ovaries, fallopian tubes, and surrounding pelvic tissues. Inflammation, scar tissue, and hormonal imbalances can interfere with egg release or embryo implantation. However, with early diagnosis and proper treatment, many women with endometriosis can still conceive successfully.
Yes. Many women with mild or moderate endometriosis conceive naturally. Maintaining a healthy lifestyle, tracking ovulation, and managing symptoms through medical supervision can improve the chances of natural conception. For others, assisted fertility treatments may be recommended.
IVF success rates for women with endometriosis vary depending on age, ovarian health, and disease severity. In general, success rates range between 30%–50% per cycle, especially when the condition is well-controlled before treatment. Consulting a fertility specialist can help determine the best approach for each individual.
Yes. Laparoscopic surgery and hormonal therapies can remove or control endometrial growths, restore pelvic anatomy, and improve ovulation. These treatments often increase the likelihood of natural conception or enhance the success of assisted reproductive methods like IVF or IUI.
A balanced anti-inflammatory diet can support hormonal health and reduce endometriosis symptoms. Including foods rich in omega-3s, fiber, and antioxidants – while limiting processed and high-sugar foods – may positively impact fertility outcomes and overall well-being.
Author
-

Dr. Smeet, true to his name, is known for his warm personality and cheerful smile that make patients instantly feel at ease with him.
Until now, he has performed 8000+ surgeries and several of which are supra-major surgeries for deep infiltrating endometriosis and fertility enhancing surgeries. With several publications in notable journals, he is constantly pushing the envelope of possibilities in gynecological surgeries