Endometriosis and pregnancy are often discussed together because the condition can complicate both conception and the journey of carrying a child. Endometriosis is a chronic gynecological condition where tissue similar to the uterine lining grows outside the uterus, causing pain, inflammation, and sometimes infertility. For women planning to start a family, it raises questions such as “Can you get pregnant with endometriosis?”, “What are the risks during pregnancy?”, and “Does pregnancy cure endometriosis?”
This blog aims to provide an evidence-based, patient-friendly guide on how endometriosis interacts with pregnancy. From understanding the condition’s impact on fertility to exploring miscarriage risks, pregnancy complications, safe management, and postpartum care, we’ll cover everything you need to know. You’ll also learn practical steps for reducing risks, real-life endometriosis pregnancy success stories, and why seeking specialist support at a trusted hospital like Mayflower can make the journey smoother and safer.
By the end, you will have a clearer understanding of how to manage endometriosis and pregnancy together-with hope, preparation, and the right medical care.
Understanding Endometriosis and Pregnancy
Endometriosis affects nearly 10% of reproductive-age women worldwide, and many only discover it when they face challenges conceiving. The condition occurs when endometrial-like tissue grows outside the uterus, leading to inflammation, adhesions, and scarring. These changes can interfere with the reproductive system, affecting ovulation, fertilization, and implantation.
Pregnancy with endometriosis is possible, but it requires careful monitoring because of higher risks compared to women without the condition. Women often wonder if pregnancy itself can “heal” endometriosis or make symptoms disappear. While some symptoms may improve temporarily due to hormonal changes, endometriosis remains a chronic condition that may return after delivery.
At Mayflower Hospital, our specialists emphasize that endometriosis and pregnancy are best managed with a personalized approach-starting before conception, continuing through each trimester, and extending into postpartum care. With early diagnosis, evidence-led treatment, and compassionate medical support, women with endometriosis can still achieve healthy pregnancies.
What is Endometriosis and How It Affects Conception
Endometriosis is not just a condition of pelvic pain-it directly impacts fertility. Adhesions can distort pelvic anatomy, ovarian cysts (endometriomas) can reduce ovarian reserve, and chronic inflammation can affect egg quality. For women asking “Can you get pregnant with endometriosis?”, the answer is yes, but the chances depend on the severity of the disease and timely medical interventions.
Why Pregnancy with Endometriosis Needs Specialized Monitoring
Endometriosis increases risks such as miscarriage, preterm labor, and complications during delivery. Regular scans, nutritional support, and specialist care are crucial to ensure mother and baby stay safe. Early engagement with a gynecologist experienced in both endometriosis and high-risk pregnancies can make a significant difference.
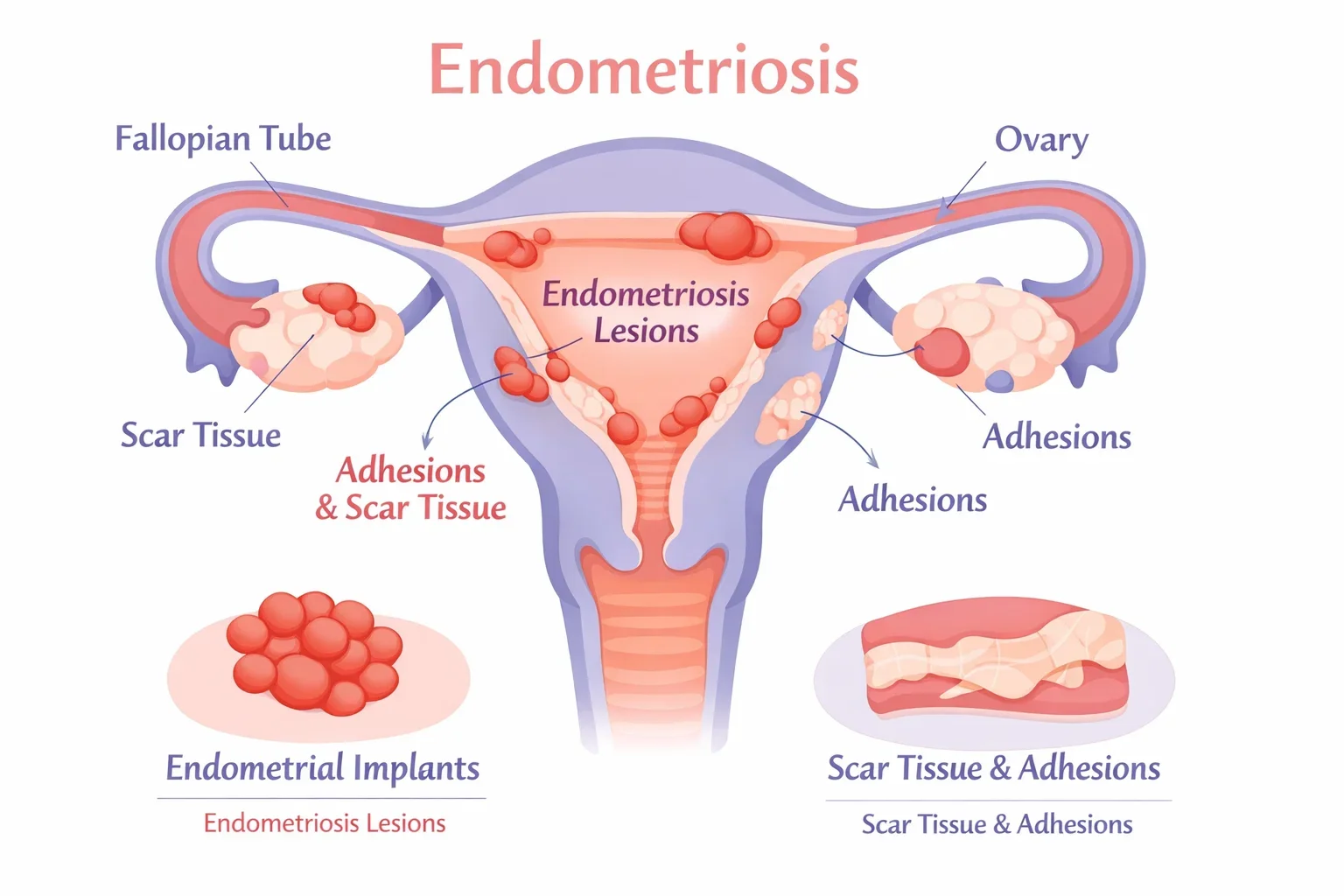
Adhesions, Inflammation, and Ovarian Endometriomas
- Adhesions: Bands of scar tissue that can restrict reproductive organs.
- Inflammation: Creates a hostile environment for egg and sperm interaction.
- Endometriomas: “Chocolate cysts” on the ovaries that may affect ovarian function.
These mechanisms explain why endometriosis can delay conception and why pregnancy requires structured follow-up at every stage.
Can You Get Pregnant with Endometriosis?
One of the most common questions women ask is, “Can you get pregnant with endometriosis?” The answer is yes, many women with endometriosis do conceive naturally or with medical support. However, fertility challenges are more likely compared to women without the condition. Endometriosis can reduce the chances of natural conception by affecting the ovaries, fallopian tubes, and uterine environment.
While some women experience minimal difficulty, others may require fertility assistance such as intrauterine insemination (IUI) or in-vitro fertilization (IVF). The important thing to remember is that having endometriosis does not mean pregnancy is impossible-it simply means it may take longer or need guided treatment.
Natural Conception vs. Time-to-Pregnancy
Studies suggest that women with mild endometriosis can achieve natural conception within one year of trying, although the time-to-pregnancy is often longer. For women with moderate to severe disease, adhesions and ovarian cysts can make natural conception more difficult. In such cases, seeking early fertility counseling improves outcomes.
When to Consider IUI or IVF (Stage-Wise Guidance)
- Mild cases (Stage I–II): Natural conception is possible; fertility treatments are usually considered if pregnancy does not occur after 6–12 months.
- Moderate cases (Stage III): Fertility treatments such as IUI may be recommended, especially if adhesions or ovarian cysts are present.
- Severe cases (Stage IV): IVF is often the most effective option, particularly when both fallopian tubes are affected or surgery has reduced ovarian reserve.
Pre-Conception Optimization
Before trying to conceive, women with endometriosis can improve their chances by:
- Maintaining a healthy weight through diet and exercise.
- Taking prenatal vitamins (folic acid, vitamin D, iron).
- Managing pain carefully under medical supervision.
- Considering laparoscopic surgery for severe disease if advised by a gynecologist.
These proactive steps improve fertility outcomes and make pregnancy safer.
Endometriosis Pregnancy Risks
Pregnancy with endometriosis requires closer medical supervision because women face a higher likelihood of complications compared to those without the condition. Research shows that endometriosis pregnancy risks include miscarriage, preterm birth, gestational hypertension, placenta complications, and a higher rate of C-sections. Understanding these risks helps women prepare and doctors plan proactive care strategies.

Endometriosis Miscarriage Risk
Several studies indicate that women with endometriosis have a slightly higher miscarriage risk, particularly during the first trimester. This may be due to inflammation in the uterine lining and poor implantation of the embryo. Early and regular ultrasounds are important for tracking pregnancy progression.
Preventive strategies include preconception counseling, optimizing health before conception, and close monitoring during the early weeks. Emotional support is equally vital, as fear of miscarriage can increase stress levels, which may indirectly affect pregnancy well-being.
Endometriosis Pregnancy Complications
Beyond miscarriage, endometriosis can cause complications later in pregnancy, such as:
- Preterm labor: Higher chance of delivering before 37 weeks.
- Placenta previa: Placenta covers part of the cervix, making natural delivery difficult.
- Gestational hypertension & preeclampsia: Increased risk due to inflammation.
- Small-for-gestational-age infants: Restricted fetal growth due to impaired blood supply.
- C-section likelihood: Adhesions and pelvic scarring increase chances of surgical delivery.
Ectopic Pregnancy and Endometriosis
Women with endometriosis are at slightly higher risk of ectopic pregnancy, where the embryo implants outside the uterus, often in the fallopian tube. This is a medical emergency and requires immediate care. Key warning signs include severe abdominal pain, shoulder-tip pain, fainting, and vaginal bleeding.
At Mayflower Hospital, gynecologists use early transvaginal ultrasound scans to confirm correct embryo placement and minimize the danger of ectopic pregnancies.
Trimester-Wise Care Plan
Every stage of pregnancy brings unique changes for women with endometriosis. Having a trimester-specific care plan ensures early detection of complications and personalized monitoring for both mother and baby.
First Trimester (Weeks 1–12)
The first trimester is critical because the risk of miscarriage is highest during this period. Women with endometriosis need early scans to confirm the location of the pregnancy and detect potential issues like ectopic pregnancy. Hormonal shifts may temporarily reduce endometriosis-related pain, but pelvic discomfort can still occur.
Key priorities:
- Early confirmation scan to rule out ectopic pregnancy.
- Monitoring for spotting, cramping, or unusual pain.
- Managing nausea, fatigue, and distinguishing them from endometriosis symptoms.
- Emotional reassurance and stress reduction.
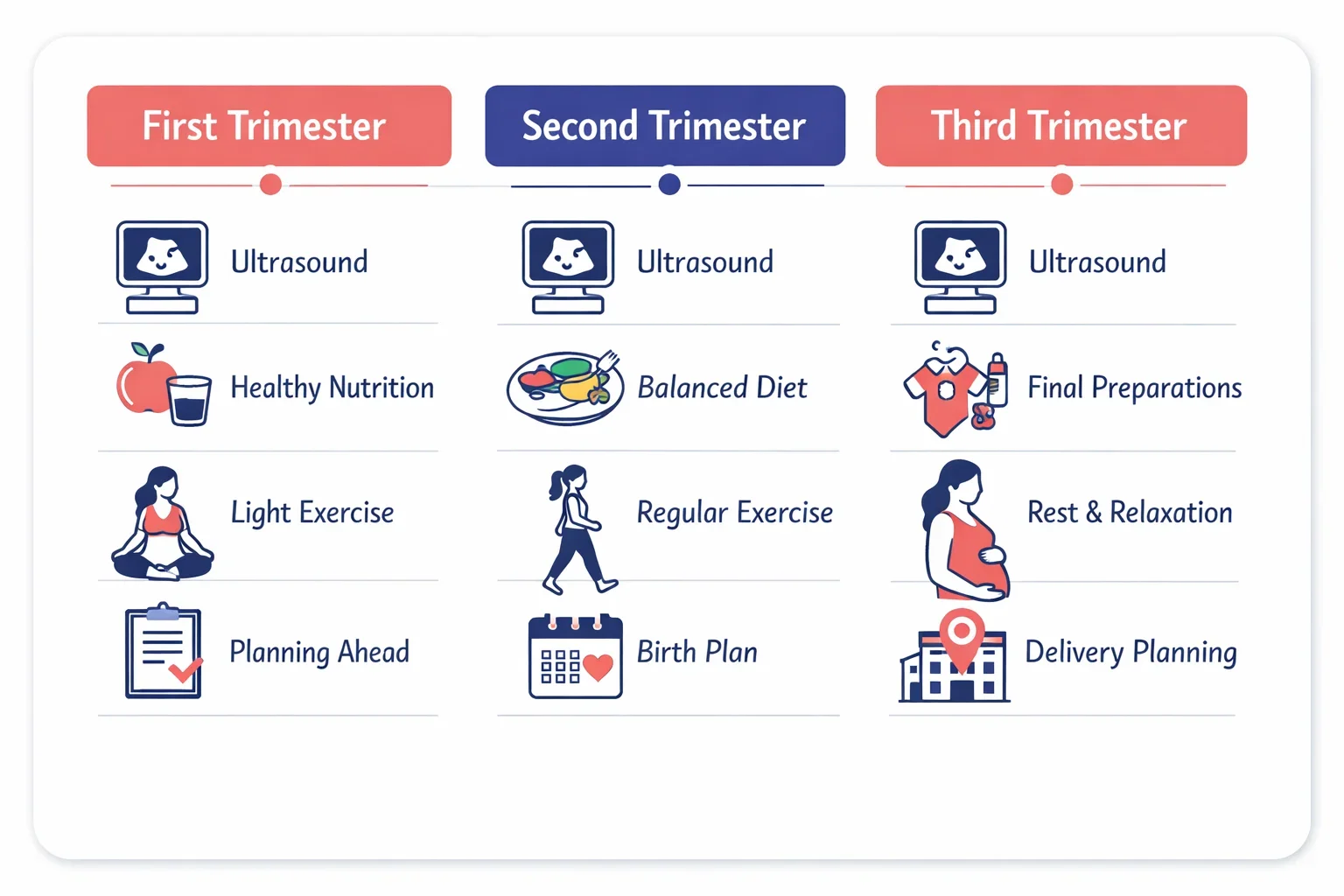
Second Trimester (Weeks 13–27)
Often called the “golden trimester,” this stage brings relief from early pregnancy symptoms. However, women with endometriosis may continue to feel pelvic pain or digestive discomfort due to adhesions. Growth scans are important to ensure the baby is developing normally.
Key priorities:
- Mid-trimester anomaly scan (18–20 weeks).
- Monitoring adhesions that may cause abdominal tightness.
- Light exercises and physiotherapy to improve posture.
- Nutritional guidance to support healthy weight gain.
Third Trimester (Weeks 28–40)
The final trimester is focused on preparing for delivery and managing rising discomforts. Women with endometriosis have a higher chance of C-sections due to adhesions and pelvic scarring, but vaginal delivery may still be possible.
Key priorities:
- Regular growth scans to monitor for restricted fetal growth.
- Assessing placenta position (to check for previa).
- Discussing birth plan with the obstetrician (normal vs. C-section).
- Monitoring for signs of preterm labor, swelling, or high blood pressure.
Visit Frequency & Key Tests per Trimester
- First trimester: Initial bloodwork, dating scan, and possible progesterone support.
- Second trimester: Anatomy scan, glucose tolerance test, blood pressure checks.
- Third trimester: Growth scans, non-stress test, blood pressure and urine monitoring for preeclampsia.
Regular checkups allow doctors to detect risks early and keep pregnancy outcomes safer.
Endometriosis Symptoms During Pregnancy
Many women hope pregnancy will ease their endometriosis symptoms, and in some cases, hormonal changes do bring relief. However, others may continue to experience discomfort, while some develop new challenges linked to both pregnancy and endometriosis. Recognizing the difference between typical pregnancy discomforts and endometriosis-related pain is essential for timely medical support.
Endometriosis Pain During Pregnancy vs. Routine Pregnancy Aches
- Endometriosis pain: Often sharp, localized pelvic or lower abdominal pain that may not improve with rest. Pain may worsen around adhesions or ovarian cysts.
- Routine pregnancy aches: Typically linked to ligament stretching, back strain, or uterine growth. These are more diffuse and improve with posture correction or rest.
If pain is persistent, severe, or associated with spotting or fever, medical evaluation is necessary to rule out complications.
When Symptom Changes Require Review
During pregnancy, endometriosis symptoms can sometimes flare due to stretching of scar tissue or hormonal fluctuations. Women should contact their doctor if they experience:
- Sudden, sharp pelvic pain that does not subside.
- Vaginal bleeding beyond light spotting.
- Pain accompanied by fever or chills.
- New digestive issues such as severe constipation or rectal bleeding.
These could indicate complications like ovarian cyst rupture, bowel involvement, or early labor-conditions that require prompt care.
Does Pregnancy Cure Endometriosis?
A common belief is that pregnancy can “cure” endometriosis. While symptoms often improve temporarily due to hormonal changes, medical research confirms that pregnancy does not cure endometriosis. After childbirth and breastfeeding, the condition may return, especially once menstrual cycles restart.
Hormonal Shift During Pregnancy
During pregnancy, estrogen levels change and progesterone levels rise. This can suppress the activity of endometrial tissue outside the uterus, which is why many women feel relief from pain during these months. However, this effect is temporary.
Why Recurrence Can Happen After Delivery
Once menstrual cycles resume postpartum, endometrial-like tissue outside the uterus may become active again. Adhesions and scarring caused by previous endometriosis do not disappear with pregnancy. For this reason, women should plan postpartum follow-ups with their gynecologist to discuss ongoing management.
Postpartum Plan to Prevent Flare-Ups
- Schedule a gynecology checkup after delivery.
- Discuss safe pain management options while breastfeeding.
- Consider hormonal therapy or contraception for long-term control if recommended.
- Focus on nutrition, stress reduction, and gradual return to activity.
Safe Pain Relief and Medication Guide
Managing pain is one of the biggest concerns for women experiencing endometriosis and pregnancy together. While some women feel relief during pregnancy, others continue to struggle with pelvic pain, cramps, or discomfort caused by adhesions. The key is to follow an evidence-led approach where pain relief options are tailored to both the mother’s and baby’s safety.

Pharmacologic Options Considered in Pregnancy
Doctors may recommend limited and carefully monitored medications to reduce pain. Some commonly considered options include:
- Acetaminophen (paracetamol): Often considered safe for short-term use.
- Limited NSAIDs: Sometimes used in early pregnancy under strict supervision, but generally avoided later due to fetal risks.
- Other pain medications: Only prescribed when benefits outweigh risks and always under gynecologist guidance.
⚠️ Important: Never self-medicate. Every drug should be cleared by your treating doctor.
Non-Pharmacologic Strategies
Many women find relief through supportive, non-drug methods, such as:
- Pelvic floor physiotherapy to ease muscle tension.
- Heat therapy using warm compresses (avoiding direct abdominal heat).
- Postural adjustments and supportive pillows to reduce strain.
- Mind-body practices such as prenatal yoga, meditation, or breathing techniques.
- Sleep hygiene to improve rest and reduce pain sensitivity.
What to Avoid Without Medical Advice
- Herbal remedies or over-the-counter supplements not approved by your doctor.
- Strong NSAIDs, opioids, or hormonal medications unless specifically advised.
- Prolonged use of heating pads directly over the abdomen.
Managing Endometriosis During Pregnancy
While there is no single formula to eliminate discomfort, women with endometriosis and pregnancy can significantly reduce risks by following a structured management plan. This combines lifestyle changes, medical supervision, and proactive monitoring to keep both mother and baby safe.
Diet and Lifestyle Adjustments
A balanced diet rich in fiber, lean protein, and anti-inflammatory foods can help manage bloating and discomfort. Staying hydrated prevents constipation, which is often aggravated by both pregnancy and endometriosis. Gentle physical activity such as walking, swimming, or prenatal yoga supports circulation and reduces stiffness.
Monitoring Schedule with a Gynecologist
Frequent checkups are essential because women with endometriosis may need closer observation than standard pregnancies. Doctors usually recommend:
- Regular ultrasounds to monitor growth and placenta health.
- Blood pressure monitoring to prevent preeclampsia.
- Pain reviews to distinguish normal pregnancy discomfort from endometriosis complications.
- Specialist input from fetal medicine experts when needed.
Emotional and Mental Well-Being
Living with endometriosis during pregnancy can cause anxiety. Support from family, counseling sessions, or joining a support group can ease mental stress. Hospitals like Mayflower also provide access to psychologists who specialize in pregnancy-related emotional health.
Red Flags: When to Call Your Doctor or Visit Emergency
Even with the best care, complications can arise during pregnancy with endometriosis. Knowing when to seek urgent medical attention can protect both mother and baby. Women should never ignore sudden or severe symptoms, as they may indicate miscarriage, ectopic pregnancy, or other high-risk complications.
Key Warning Signs
- Severe, one-sided abdominal pain that does not subside with rest.
- Heavy vaginal bleeding or clots, especially in the first trimester.
- Persistent fever or chills, which could suggest infection.
- Sudden swelling in the hands, feet, or face (possible preeclampsia).
- Dizziness, fainting, or severe headaches that do not improve.
- Decreased or no fetal movements in the later stages of pregnancy.
What to Share with Your Doctor
When contacting your gynecologist or visiting the emergency department, be prepared to share:
- How many weeks pregnant you are.
- The nature, intensity, and duration of pain or bleeding.
- Any associated symptoms such as nausea, fever, or fainting.
- Medications or supplements currently being used.
Clear communication helps doctors respond quickly and plan the right treatment.
Delivery Planning with Endometriosis
Planning the mode of delivery is an important part of pregnancy management for women with endometriosis. Adhesions, ovarian cysts, and pelvic scarring can influence whether vaginal birth is possible or if a C-section is safer. Discussing delivery options early helps reduce anxiety and ensures a smoother birth experience.
Vaginal Birth vs. C-Section
- Vaginal birth: Many women with mild endometriosis can deliver naturally if there are no additional complications.
- C-section: More common in women with extensive adhesions, deep pelvic endometriosis, or placenta complications. A planned C-section allows the medical team to prepare for challenges related to scar tissue.
Your obstetrician will assess factors like placenta position, baby’s growth, and maternal health before recommending the delivery method.
Anesthesia and Adhesions
Adhesions caused by endometriosis may affect the safety and ease of anesthesia during a C-section. This is why pre-anesthesia evaluation is recommended. At Mayflower Hospital, anesthesiologists collaborate closely with gynecologists to minimize risks and ensure mother and baby remain stable throughout the procedure.
Preparing Your Birth Plan
- Discuss delivery preferences early in the third trimester.
- Keep flexible options depending on baby’s position and health.
- Plan pain management strategies, including epidural anesthesia.
- Ensure your partner or support person understands possible changes in the plan.
Postpartum: Recovery, Recurrence, Breastfeeding & Contraception
The postpartum period is just as important as pregnancy when it comes to endometriosis care. While some women enjoy a temporary break from symptoms, others notice flare-ups once their menstrual cycle returns. Planning postpartum recovery and contraception with your gynecologist helps reduce complications and improve long-term well-being.
Pain and Flare-Up Prevention After Delivery
Endometriosis-related pain may return after childbirth, especially if periods resume early. Regular follow-ups with your doctor ensure timely management. Gentle exercises, pelvic floor therapy, and anti-inflammatory foods can help reduce discomfort during recovery.
Breastfeeding Considerations
Breastfeeding can delay the return of periods, sometimes helping suppress endometriosis symptoms temporarily. However, it is not a guaranteed method of disease control. Mothers should focus on adequate nutrition and hydration to support both lactation and recovery.
Contraception Choices with Endometriosis
Choosing the right contraception postpartum is important for managing both family planning and endometriosis symptoms. Options include:
- Hormonal IUDs: May help control bleeding and reduce recurrence.
- Combined hormonal pills: Not suitable for everyone during breastfeeding but effective in reducing symptoms.
- Barrier methods: Safe but do not impact endometriosis activity.
Planning Future Fertility Safely
For women considering another pregnancy, discussing timelines with a gynecologist ensures optimal spacing between births. Fertility treatments may be recommended earlier if recurrence affects conception.
Endometriosis Pregnancy Success Stories
Hearing real-life journeys can be deeply reassuring for women navigating endometriosis and pregnancy. While the path may involve challenges, countless women with endometriosis have successfully carried healthy pregnancies with the right medical support.
Inspiring Examples
- Case 1 (Mild endometriosis): A woman diagnosed in her late twenties conceived naturally within a year after making lifestyle adjustments and following regular checkups. She went on to deliver a healthy baby through normal delivery.
- Case 2 (Moderate endometriosis): After laparoscopic surgery and a few cycles of IUI, a couple achieved pregnancy. With careful monitoring, the pregnancy progressed smoothly, and the mother delivered at term via C-section.
- Case 3 (Severe endometriosis): IVF was the chosen path for a woman with advanced adhesions. Despite initial fears, close monitoring and personalized treatment led to the birth of a healthy baby.
Key Takeaway
Success looks different for every woman, but modern gynecology offers many options to make parenthood possible. Whether through natural conception, surgery, or assisted reproduction, the chances of achieving a healthy pregnancy are better than ever.
Why Choose Mayflower Hospital for Endometriosis and Pregnancy Care
When it comes to managing endometriosis and pregnancy, choosing the right healthcare partner makes all the difference. At Mayflower Hospital, our team combines advanced medical expertise with compassionate care, ensuring that every woman receives a personalized plan from preconception to postpartum recovery.
Multidisciplinary Team of Specialists
Mayflower brings together gynecologists, laparoscopic surgeons, fertility experts, anesthesiologists, and fetal medicine specialists. This collaborative approach ensures that every stage-conception, pregnancy monitoring, delivery, and recovery-is handled with precision and safety.
Advanced Facilities and Evidence-Led Care
Our hospital is equipped with state-of-the-art diagnostic tools, advanced laparoscopic surgery suites, and dedicated high-risk pregnancy monitoring units. Women receive care that is aligned with international guidelines, including those from ASRM and ACOG, ensuring optimal outcomes for both mother and baby.
Integrated Pathway for Long-Term Support
From preconception counseling to maternity care, and from delivery to postpartum follow-up, Mayflower offers an integrated pathway that reduces anxiety and builds trust. Patients receive not only medical treatment but also emotional and psychological support to navigate the journey.
Checklist: Planning Pregnancy with Endometriosis
Preparing for pregnancy with endometriosis requires extra attention to health, timing, and medical guidance. Use this checklist to stay organized and proactive.
Before Conception
- Schedule a gynecology consultation for personalized guidance.
- Consider laparoscopy or fertility evaluation if you’ve been trying >6–12 months.
- Begin prenatal vitamins, including folic acid, vitamin D, and iron.
- Focus on weight management and anti-inflammatory nutrition.
- Discuss safe pain management strategies with your doctor.
During Pregnancy
- Attend all scheduled antenatal visits and scans.
- Track pain patterns and report any unusual symptoms early.
- Stay hydrated and include fiber to avoid constipation.
- Practice light, safe exercise such as walking or prenatal yoga.
- Prepare a flexible birth plan with your obstetrician.
Postpartum & Beyond
- Schedule a postpartum review to plan long-term endometriosis management.
- Explore breastfeeding benefits and contraception options.
- Consider future fertility plans and timelines with your doctor.
Myths vs Facts
Misinformation about endometriosis and pregnancy often increases stress and confusion. Here’s a simple comparison to set the record straight:
| Myth | Fact |
|---|---|
| Pregnancy cures endometriosis. | Pregnancy may reduce symptoms temporarily, but endometriosis often returns after delivery. |
| Women with endometriosis cannot get pregnant. | Many women conceive naturally or with support such as IUI/IVF. |
| All pregnancies with endometriosis are high-risk. | Risks are higher, but with close monitoring, many pregnancies progress smoothly. |
| C-section is the only delivery option. | Vaginal delivery is possible for many women unless complications require surgery. |
| Pain during pregnancy is always normal. | Persistent or severe pain should be assessed by a doctor to rule out complications. |
Conclusion
Navigating endometriosis and pregnancy can feel overwhelming, but with the right medical support, many women achieve safe and healthy outcomes. While the condition brings higher risks of miscarriage, pain, and delivery complications, these challenges can be managed with early planning, regular monitoring, and specialist care.
Pregnancy may not cure endometriosis, but it does not prevent women from becoming mothers. With lifestyle adjustments, fertility support when needed, and trimester-wise medical supervision, positive results are within reach.
At Mayflower Hospital, our multidisciplinary team is dedicated to guiding women every step of the way-from conception to postpartum recovery. If you are living with endometriosis and planning pregnancy, a personalized care plan can make your journey safer and more reassuring.
FAQs on Endometriosis and Pregnancy
Yes, many women with endometriosis conceive naturally or with fertility support. While it may take longer in some cases, treatments such as IUI or IVF improve chances of conception.
Women with endometriosis face a slightly higher miscarriage risk, especially in the first trimester. Regular scans and early monitoring help detect problems quickly and reduce complications.
No, pregnancy does not cure endometriosis. Symptoms may improve temporarily due to hormonal changes, but the condition often returns after delivery.
Mild pain can be managed with safe medications such as acetaminophen, along with non-drug strategies like physiotherapy, warm compresses, and prenatal yoga. Always consult your gynecologist before taking any medication.
Women with endometriosis have a higher risk of preterm birth, placenta previa, gestational hypertension, and C-section deliveries. With proper care, most of these risks can be managed effectively.
IVF is often recommended for women with severe endometriosis, blocked fallopian tubes, or those who have not conceived naturally after 6–12 months of trying.
Yes, vaginal birth is possible for many women. However, adhesions and scarring may sometimes make a C-section safer. Your doctor will decide based on your individual case.
Author
-

Dr. Smeet, true to his name, is known for his warm personality and cheerful smile that make patients instantly feel at ease with him.
Until now, he has performed 8000+ surgeries and several of which are supra-major surgeries for deep infiltrating endometriosis and fertility enhancing surgeries. With several publications in notable journals, he is constantly pushing the envelope of possibilities in gynecological surgeries