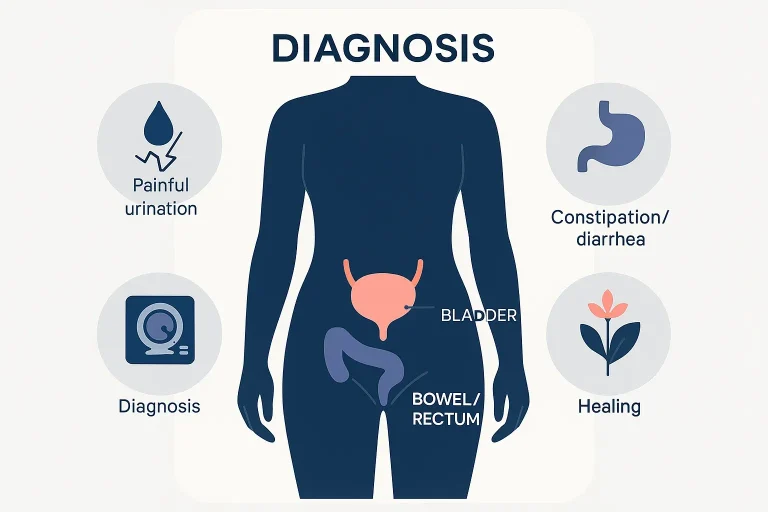
Endometriosis bladder symptoms are among the most overlooked aspects of women’s health, often misdiagnosed as simple urinary infections or digestive issues. In reality, endometriosis is a chronic condition where tissue similar to the uterine lining grows outside the uterus. When this tissue affects the bladder or bowel, the results can be painful, disruptive, and confusing. Many women experience endometriosis bowel symptoms alongside urinary issues, creating a double burden that impacts not just physical health but also mental well-being and quality of life.
The link between endometriosis and urinary or bowel problems is complex. Symptoms may include painful urination in endometriosis, urinary urgency, constipation, diarrhea, or even rectal bleeding. These warning signs often overlap with conditions such as urinary tract infections (UTIs) or irritable bowel syndrome (IBS), making diagnosis difficult. Unfortunately, this delay often leads to years of unnecessary suffering before the right treatment begins.
At Mayflower Women’s Hospital, we believe that timely recognition and treatment of bladder endometriosis and bowel endometriosis can transform a patient’s life. Our multidisciplinary team combines advanced imaging, minimally invasive surgery, and evidence-based therapies to offer comprehensive care. Whether you are seeking clarity on unexplained urinary pain or exploring bowel endometriosis treatment, this guide will explain symptoms, causes, diagnostic methods, and treatment pathways.
By the end of this blog, you will understand:
- How endometriosis affects the bladder and bowel
- The difference between bowel endometriosis symptoms vs IBS
- Available treatments, from medication to bowel endometriosis surgery
- Why specialized centers like Mayflower provide the best outcomes
What Are Endometriosis Bladder Symptoms?
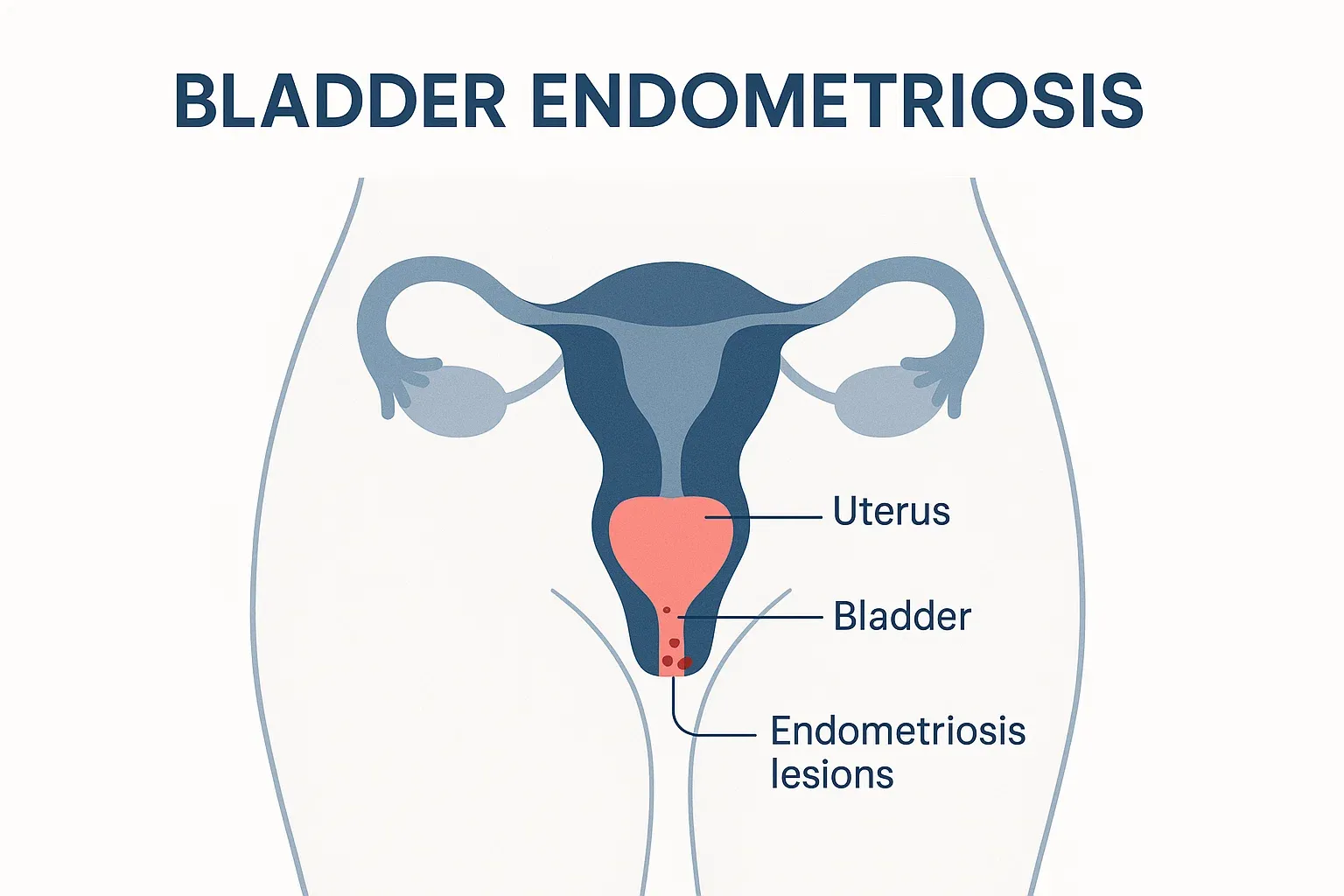
Endometriosis can directly affect the bladder when tissue implants form on or within its wall. Known as bladder endometriosis, this condition is rare but often underdiagnosed. Because the symptoms closely resemble those of common urinary tract infections, many women go through repeated antibiotic courses without relief. Recognizing the unique pattern of symptoms is the first step toward proper care.
Common Urinary Symptoms of Endometriosis
Women with bladder involvement often report:
- Frequent urination – needing to pass urine more often, even at night.
- Urgency – a sudden, strong urge to urinate that is difficult to control.
- Painful urination endometriosis – burning or cramping pain during urination, especially around menstruation.
- Blood in urine – occasional hematuria (blood in urine), particularly during periods.
- Pelvic pain – ongoing discomfort around the bladder area that worsens with a full bladder.
These symptoms, when cyclical and linked with menstrual cycles, strongly suggest urinary symptoms of endometriosis rather than a simple infection.
Overlap With Urinary Tract Infections
Many patients are initially treated for UTIs because the complaints are similar. However, bladder endometriosis has distinguishing features:
- Symptoms worsen during periods.
- Antibiotics do not provide lasting relief.
- Pain may spread to the pelvis or lower back.
This overlap often delays proper evaluation, which is why awareness is critical.
How Bladder Endometriosis Is Diagnosed
A timely bladder endometriosis diagnosis can prevent complications. Doctors may use:
- Pelvic ultrasound to detect abnormalities.
- MRI scans for a detailed view of pelvic organs.
- Cystoscopy, where a camera is inserted into the bladder to check for lesions.
- Laparoscopy, the gold standard, to confirm and sometimes treat the condition.
Early detection is important because untreated bladder lesions can deepen and compromise bladder function.
Just as the bladder can be affected by endometriosis, so too can the intestines. Next, we will look at the range of endometriosis bowel symptoms, how they differ from IBS, and why they are often misunderstood.
Endometriosis Bowel Symptoms to Watch
When endometrial tissue attaches to the intestines or rectum, it is called bowel endometriosis. This form affects nearly 10–15% of women with advanced endometriosis and can be one of the most disruptive types because it interferes with digestion and bowel movements. Unlike simple digestive issues, these symptoms often worsen around menstruation, making them cyclical in nature.
Common Signs of Bowel Endometriosis
Women may experience:
- Painful bowel movements – cramping or sharp pain during defecation, especially in the days leading up to and during periods.
- Constipation and diarrhea – alternating bowel changes that mimic IBS.
- Rectal bleeding – spotting or blood in stool, often mistaken for hemorrhoids.
- Bloating and abdominal swelling – commonly referred to as “endo belly.”
- Deep pelvic pain – discomfort during sex or prolonged sitting, linked to lesions near the rectum.
These symptoms not only cause physical discomfort but also disrupt daily life and social activities, leading many women to silently suffer.
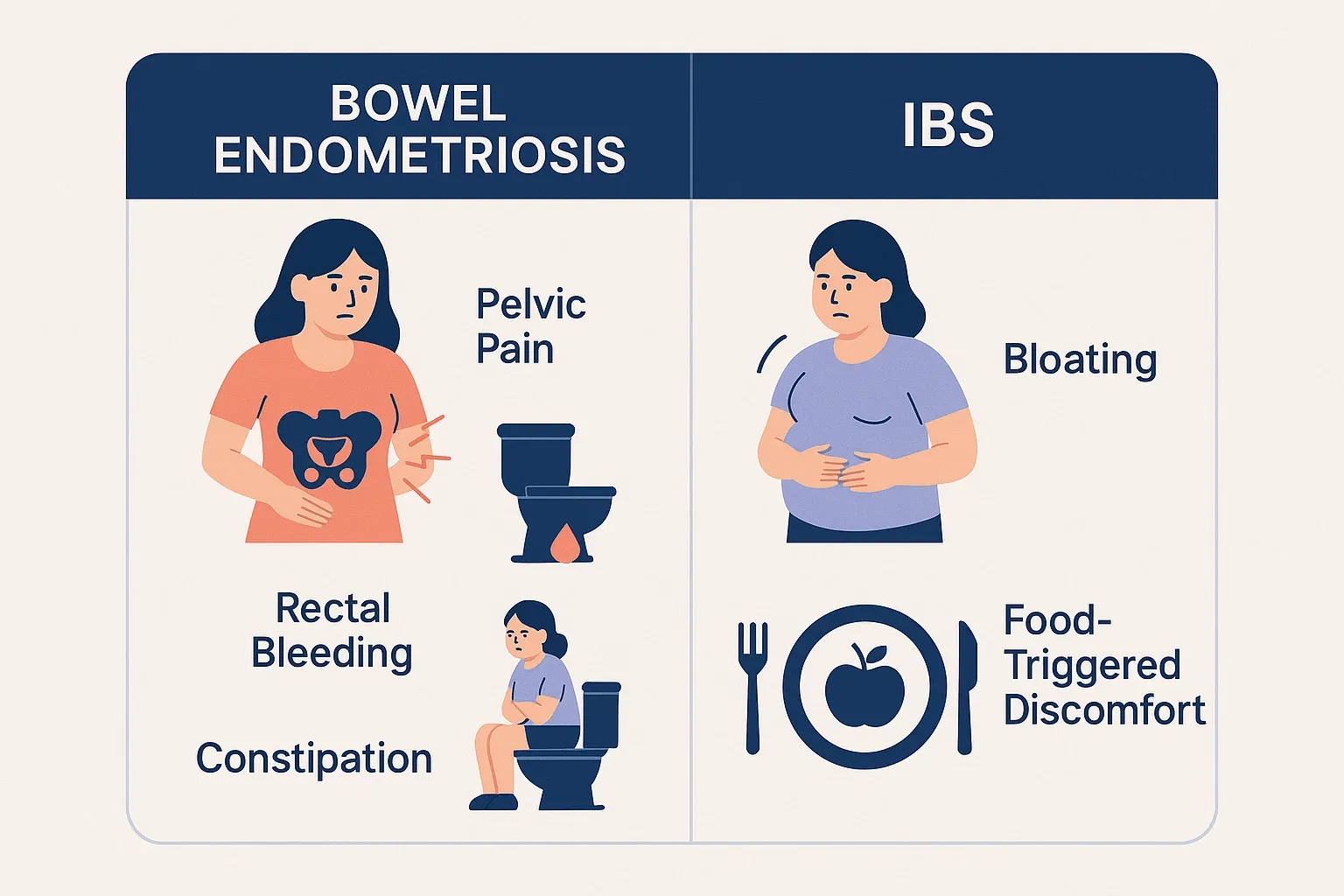
Bowel Endometriosis Symptoms vs IBS
One of the biggest diagnostic challenges is distinguishing bowel endometriosis symptoms vs IBS (Irritable Bowel Syndrome). Both conditions share bloating, irregular bowel habits, and abdominal pain. However, there are key differences:
| Feature | Bowel Endometriosis | IBS |
| Pain pattern | Cyclical, worse during periods | Non-cyclical, stress or diet-related |
| Associated symptoms | Pelvic pain, painful sex, infertility | Gas, food intolerances, stress triggers |
| Bleeding | Possible rectal bleeding during menstruation | Rare |
| Response to treatment | May improve with hormones or surgery | Improves with diet/stress management |
This comparison highlights why patients who have both digestive and gynecological symptoms should undergo thorough evaluation.
When to Suspect Rectovaginal Endometriosis
In severe cases, endometriosis infiltrates the space between the rectum and vagina, known as rectovaginal endometriosis. This often causes:
- Severe pain during intercourse
- Pain when passing stool
- Sensation of obstruction in the rectum
- Bleeding from the rectum during periods
These advanced cases usually require surgical expertise for proper treatment.
Now that we’ve explored bladder and bowel symptoms individually, the next step is to understand why these complications occur in endometriosis and how the disease spreads to such critical organs.
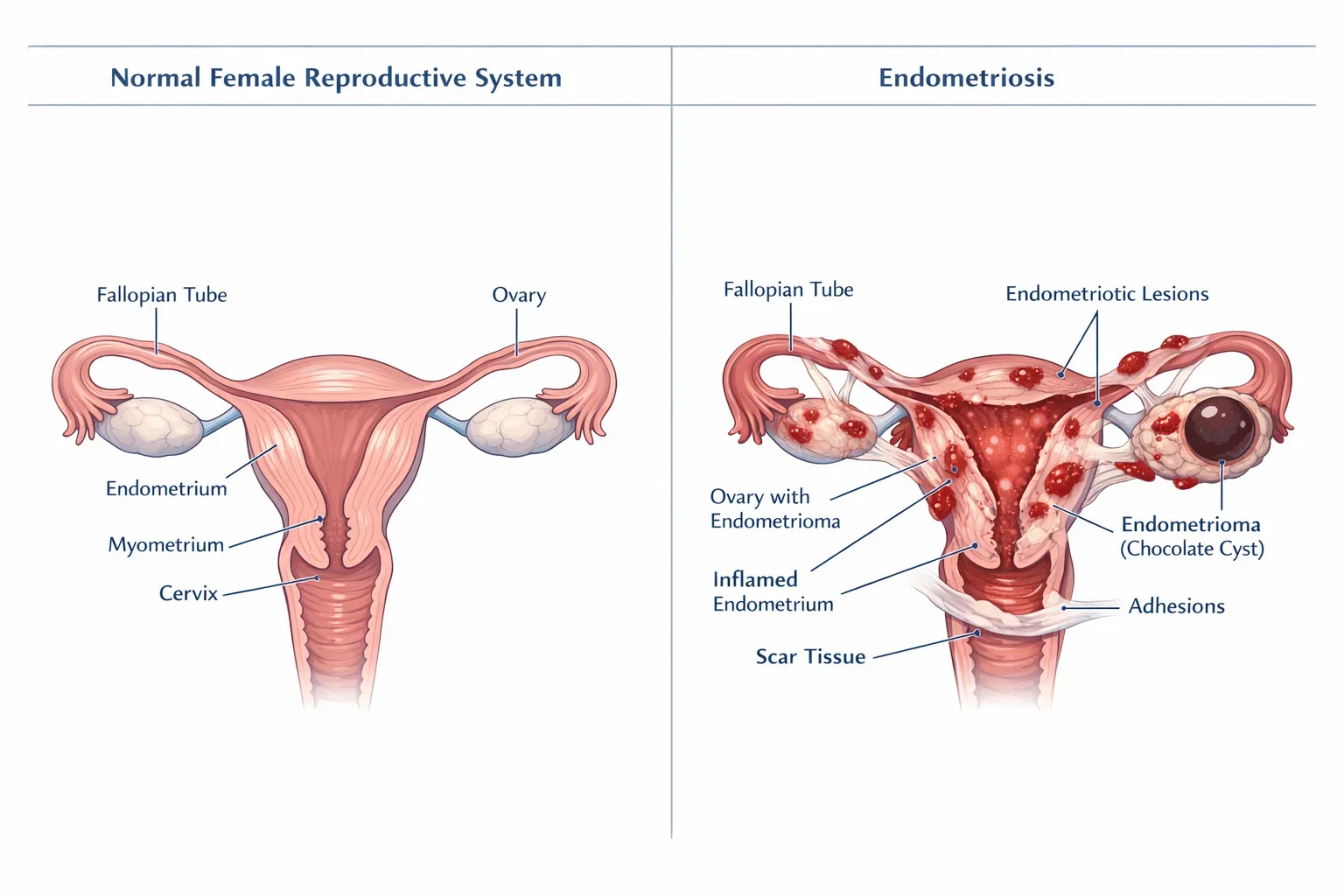
Why Do Bladder and Bowel Symptoms Happen in Endometriosis?
Endometriosis is not confined to the uterus. The condition occurs when tissue resembling the endometrium grows outside its normal location and responds to hormonal cycles. Over time, these growths can extend to nearby pelvic organs like the bladder, rectum, and intestines. When this happens, symptoms become more complex and difficult to manage.
How Endometrial Tissue Affects the Bladder
When endometrial implants form on the bladder surface or invade its wall, they create inflammation and scarring. This explains the classic urinary symptoms of endometriosis, such as frequent urination, urgency, or painful urination. In some cases, scar tissue (adhesions) may cause the bladder to stick to the uterus, intensifying pelvic pain.
Mechanisms Behind Bowel Endometriosis
Bowel endometriosis occurs when these implants grow on the rectum, sigmoid colon, or small intestines. During menstruation, the tissue bleeds internally, leading to irritation and swelling. Over time, this causes narrowing of the bowel, painful bowel movements, and in advanced cases, partial obstruction. The cyclical nature of these symptoms is the strongest indicator that endometriosis is the root cause rather than IBS or dietary intolerance.
Rectovaginal Endometriosis – The Most Severe Form
Among the most challenging cases is rectovaginal endometriosis, where tissue grows deep between the vagina and rectum. This form often causes severe pain during intercourse, chronic constipation, and rectal bleeding during periods. Because of its location, it requires careful surgical planning and the expertise of a multidisciplinary team.
Why These Symptoms Are Often Misunderstood
Bladder and bowel symptoms of endometriosis are frequently overlooked because they mimic other conditions. Many women undergo repeated treatments for UTIs, IBS, or hemorrhoids without relief. Delays in diagnosis not only worsen symptoms but also affect fertility and long-term pelvic health.
Understanding the cause of these symptoms highlights the importance of accurate evaluation. Next, we will explore how doctors perform a bladder endometriosis diagnosis and the treatment options available.
Bladder Endometriosis Diagnosis and Treatment Options
Bladder endometriosis is challenging to identify because its symptoms are often mistaken for urinary tract infections or interstitial cystitis. However, accurate diagnosis is essential for effective treatment and long-term relief. At Mayflower Women’s Hospital, our specialists use advanced imaging and minimally invasive approaches to detect and manage this condition.

How Doctors Diagnose Bladder Endometriosis
Diagnosis usually follows a stepwise approach:
- Medical history and symptom tracking – Identifying patterns, especially urinary pain linked to menstruation.
- Pelvic ultrasound – Useful for detecting larger nodules or associated ovarian cysts.
- MRI scan – Provides detailed images of the bladder wall and surrounding tissues.
- Cystoscopy – A small camera inserted into the bladder to directly visualize lesions.
- Laparoscopy – The gold standard that allows confirmation and immediate treatment of lesions.
A timely bladder endometriosis diagnosis prevents the progression of disease and reduces the risk of bladder dysfunction.
Medical Management
For women with mild symptoms, medications may help reduce pain and control disease progression. Options include:
- Hormonal therapy – Birth control pills, progestins, or GnRH analogues to suppress menstruation and shrink lesions.
- Pain relief medications – Nonsteroidal anti-inflammatory drugs (NSAIDs) for symptom relief.
While these options provide temporary relief, they do not eliminate lesions.
Surgical Options
When bladder involvement is severe, surgery may be required. Approaches include:
- Laparoscopic excision – Removal of surface implants with minimal scarring.
- Partial cystectomy – In rare cases, removal of a small bladder section if lesions are deep.
These procedures are highly specialized and should be performed by experienced surgeons, as they aim to restore normal bladder function while preserving surrounding tissues.
Role of a Multidisciplinary Team
Bladder endometriosis often coexists with bowel or reproductive involvement. A multidisciplinary approach — involving gynecologists, urologists, and radiologists — ensures precise treatment planning. At Mayflower, our endometriosis experts collaborate to deliver safe and comprehensive care tailored to each woman’s needs.
Just as the bladder can be treated with medical and surgical methods, the bowel requires specialized approaches. Next, we will discuss bowel endometriosis treatment options, including surgery and lifestyle support.
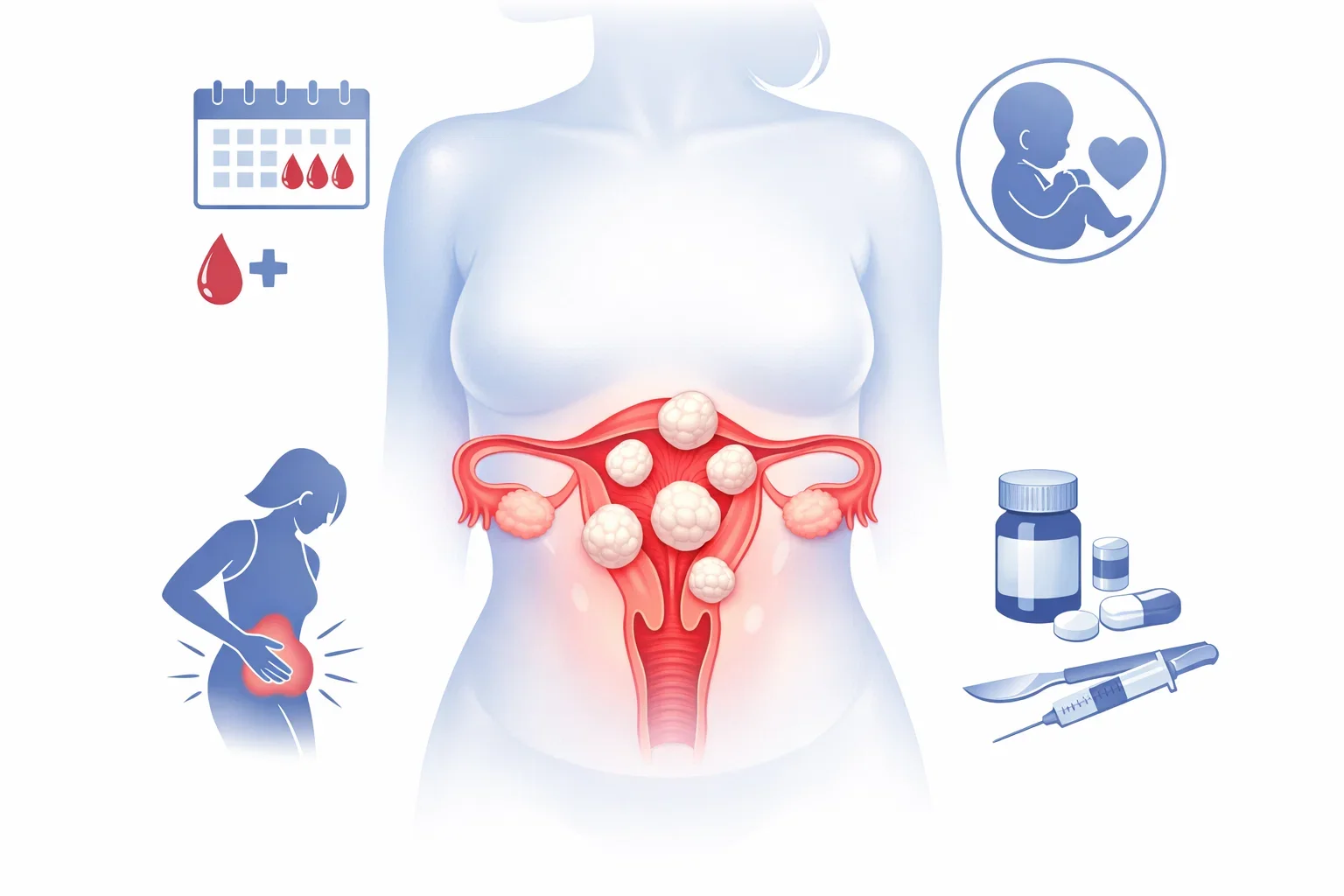
Bowel Endometriosis Treatment Approaches
Managing bowel endometriosis requires a combination of medical therapies and surgical precision. Because the condition can significantly affect digestion, pelvic comfort, and fertility treatment plans must be highly individualized. At Mayflower Women’s Hospital, our multidisciplinary approach ensures that women receive tailored care, ranging from medication to advanced surgical interventions.
Medical Therapy for Bowel Endometriosis
In the early stages or for women who cannot undergo surgery immediately, medical management can help:
- Hormonal therapy – Birth control pills, progestins, or GnRH analogues to reduce lesion activity and ease pain.
- Pain management – NSAIDs and other pain relievers to control chronic pelvic pain.
- Dietary and lifestyle support – Anti-inflammatory diets, stress reduction, and pelvic floor physiotherapy to complement medical care.
While medications ease symptoms, they do not remove bowel lesions entirely, making surgery necessary in more advanced cases.
When Is Bowel Endometriosis Surgery Needed?
Bowel endometriosis surgery is recommended when:
- Symptoms are severe and persistent.
- Bowel obstruction or narrowing is detected.
- Rectal bleeding occurs regularly.
- Rectovaginal endometriosis invades deeper tissues.
Surgical techniques include:
- Shaving excision – Removal of superficial lesions.
- Disc resection – Cutting out part of the bowel wall where lesions are located.
- Segmental resection – Removing a diseased bowel segment and reconnecting healthy sections.
These minimally invasive procedures, performed laparoscopically, ensure faster recovery, less pain, and improved fertility outcomes.
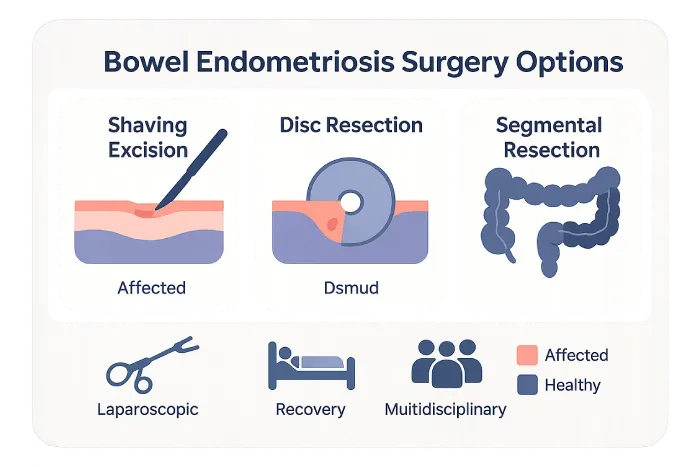
Importance of Specialized Care
Because bowel surgery requires both gynecological and gastrointestinal expertise, it is essential to be treated in a center with multidisciplinary specialists. At Mayflower, our gynecologists collaborate with colorectal surgeons and radiologists to deliver safe, effective outcomes. This integrated care model ensures that women receive not only symptom relief but also long-term improvement in quality of life.
Mayflower Endometriosis Bowel Care
Our Mayflower endometriosis bowel care program emphasizes:
- Accurate imaging and early detection.
- Individualized treatment combining medication, surgery, and supportive therapies.
- Compassionate counseling for both physical and emotional well-being.
This comprehensive approach has helped countless women regain control of their health, fertility, and daily life.
While medical and surgical treatments are important, daily management plays a big role. In the next section, we will discuss strategies for living with endometriosis bladder and bowel symptoms.
Living With Endometriosis Bladder and Bowel Symptoms
Endometriosis that affects the bladder and bowel can feel overwhelming, but with the right support, women can manage symptoms and live full, active lives. Medical and surgical treatments form the foundation of care, yet day-to-day strategies also play a crucial role in improving quality of life.
Lifestyle and Self-Care Strategies
While these steps cannot cure endometriosis, they can help reduce flare-ups and discomfort:
- Anti-inflammatory diet – Focus on fresh fruits, vegetables, lean proteins, and omega-3 fats while reducing processed foods and sugar.
- Hydration – Drinking enough water helps ease urinary urgency and prevent constipation.
- Pelvic floor therapy – Specialized physiotherapy to relax tight pelvic muscles and ease urinary or bowel pain.
- Exercise and yoga – Gentle stretching, yoga, or low-impact exercise improves circulation and reduces stress-related flare-ups.
- Stress management – Mindfulness, meditation, and counseling help women cope with the mental health challenges that often accompany chronic pain.
Emotional and Mental Well-Being
The constant pain and unpredictability of endometriosis bladder symptoms and endometriosis bowel symptoms can take a toll on emotional health. Anxiety, depression, and social withdrawal are common. Building a strong support system, joining endometriosis support groups, and seeking counseling can make a significant difference.
When to Seek Medical Help
It’s important not to dismiss urinary or digestive problems as “normal.” Women should consult a specialist if they experience:
- Persistent painful urination in endometriosis
- Blood in urine or stool
- Chronic constipation or diarrhea that worsens during menstruation
- Painful intercourse or rectal pain
Early consultation prevents complications and ensures that treatment options – including hormonal therapy, bladder endometriosis diagnosis, and surgery – are explored at the right time.
For women seeking expert care, Mayflower Women’s Hospital provides advanced diagnostic tools, surgical expertise, and holistic support. The next section highlights why Mayflower is a trusted choice for endometriosis bladder and bowel care.

Why Choose Mayflower for Endometriosis Bladder and Bowel Care
Endometriosis involving the bladder and bowel requires more than routine gynecological care. It demands specialized evaluation, advanced surgical skills, and a compassionate approach to women’s health. At Mayflower Women’s Hospital, we bring all of these together under one roof, offering hope and healing for women struggling with complex symptoms.
Expertise in Advanced Diagnosis
Mayflower offers cutting-edge diagnostic methods, including pelvic MRI, high-resolution ultrasound, and laparoscopic evaluation. These tools allow us to detect bladder endometriosis, bowel endometriosis, and even advanced forms like rectovaginal endometriosis at an early stage. Accurate diagnosis ensures that women receive timely and effective treatment.
Comprehensive Treatment Options
Our specialists provide a full spectrum of therapies, from hormonal management to minimally invasive surgery. With expertise in both bladder endometriosis diagnosis and bowel endometriosis surgery, we ensure that every treatment plan is personalized to meet a woman’s unique needs.
Multidisciplinary Team Approach
Endometriosis care at Mayflower is not limited to gynecology. Our team includes urologists, colorectal surgeons, radiologists, physiotherapists, and counselors who work together to deliver complete care. This integrated approach helps women find relief not only from pain but also from the emotional burden of the disease.
Patient-Centered Care
Beyond technology and expertise, we prioritize compassion. Every woman is guided through her journey with clear communication, continuous support, and long-term follow-up. Our Mayflower endometriosis bowel care program ensures that patients feel supported at every step – from diagnosis to recovery.
If you are experiencing urinary symptoms of endometriosis or persistent bowel problems that have not responded to standard treatments, it may be time to seek specialized care. At Mayflower, we combine medical excellence with empathy to help women reclaim their health and well-being. Book a consultation today and take the first step toward lasting relief.
FAQ Section
The most frequent urinary symptoms of endometriosis include painful urination, urinary urgency, increased frequency of urination, and in some cases blood in the urine during periods. These symptoms are often mistaken for urinary tract infections but tend to worsen around menstruation, which is a key indicator of bladder endometriosis.
Distinguishing bowel endometriosis symptoms vs IBS can be challenging because both conditions involve abdominal pain, constipation, diarrhea, and bloating. However, bowel endometriosis typically follows a cyclical pattern linked to menstruation, while IBS is more influenced by stress or diet. Additionally, rectal bleeding and deep pelvic pain are more characteristic of bowel endometriosis. Imaging tests and laparoscopy help confirm the diagnosis.
Bowel endometriosis surgery is considered when symptoms are severe, unresponsive to medical therapy, or when there is evidence of bowel obstruction, rectal bleeding, or deep rectovaginal endometriosis. Depending on the extent, surgeons may perform shaving excision, disc resection, or segmental resection. At Mayflower, these procedures are performed laparoscopically to minimize recovery time and maximize outcomes.
Yes. Painful urination endometriosis can often be managed initially with medical therapies such as hormonal treatment (birth control pills, progestins, GnRH analogues) and pain relief medication. These options reduce inflammation and suppress the hormonal cycles that fuel lesion growth. However, if lesions invade the bladder wall or symptoms persist, surgical treatment may be required for lasting relief.
Choosing the right hospital for endometriosis makes a significant difference in long-term outcomes. At Mayflower Women’s Hospital, care goes beyond symptom management. Our specialists combine advanced imaging, laparoscopic expertise, and a multidisciplinary team approach to treat both bladder endometriosis and bowel endometriosis effectively. Patients benefit from early and accurate diagnosis, minimally invasive surgery when needed, and ongoing support for recovery and emotional well-being. This comprehensive model ensures that women receive not only relief from pain but also a better quality of life.
Conclusion
Endometriosis bladder symptoms and bowel complications can be life-altering, but they are often misunderstood or misdiagnosed. What may appear to be recurring urinary infections or irritable bowel syndrome could, in fact, be signs of bladder endometriosis or bowel endometriosis. Recognizing the cyclical nature of these symptoms – and seeking timely diagnosis – is the first step toward relief.
From painful urination and rectal bleeding to the challenges of rectovaginal endometriosis, every symptom deserves attention. With options ranging from medication to advanced bowel endometriosis surgery, women today have access to effective treatments that were not always possible in the past.
At Mayflower Women’s Hospital, we combine advanced imaging, minimally invasive surgical techniques, and holistic support programs to help women reclaim control over their health. Our specialists in endometriosis bladder and bowel care understand that each woman’s journey is unique – and we tailor treatment plans to ensure the best outcomes.
Through our dedicated Mayflower endometriosis bowel care program, patients receive not only advanced surgical options but also compassionate follow-up, dietary guidance, and emotional support.