Endometriosis diet plays a vital role in managing pain, reducing inflammation, and improving quality of life for women diagnosed with endometriosis. Growing scientific evidence suggests that what you eat can influence hormonal balance, immune response, and the body’s inflammatory processes — all of which directly affect endometrial tissue growth and symptoms.
Endometriosis affects millions of women globally, yet nutrition is often overlooked in treatment discussions. Recent research has revealed that dietary changes—particularly anti-inflammatory and plant-forward eating—can significantly reduce pelvic pain and bloating while supporting overall reproductive health. These studies show that including omega-3 fats, antioxidants, and fiber can help modulate estrogen levels and lessen chronic inflammation.
At Mayflower Women’s Hospital, dietary and medical care go hand in hand. Our gynecologists and nutritionists design evidence-based nutritional programs to complement clinical treatments such as hormonal therapy or laparoscopic surgery. The goal is not just symptom relief, but long-term hormonal and metabolic balance through a sustainable eating plan.
Before exploring the right foods, it’s important to understand why diet has such a strong connection to endometriosis. The next section explains the biological link between food, hormones, and inflammation, helping you build the foundation for an effective nutrition strategy.
Understanding Endometriosis and the Role of Diet
Endometriosis is a chronic inflammatory condition in which tissue similar to the lining of the uterus grows outside it—commonly on the ovaries, fallopian tubes, and pelvic walls. This misplaced tissue reacts to hormonal changes during the menstrual cycle, leading to pain, inflammation, and sometimes fertility issues. While medical treatment is vital, the diet for endometriosis has emerged as a complementary approach that can significantly impact how the body manages inflammation and hormonal balance.
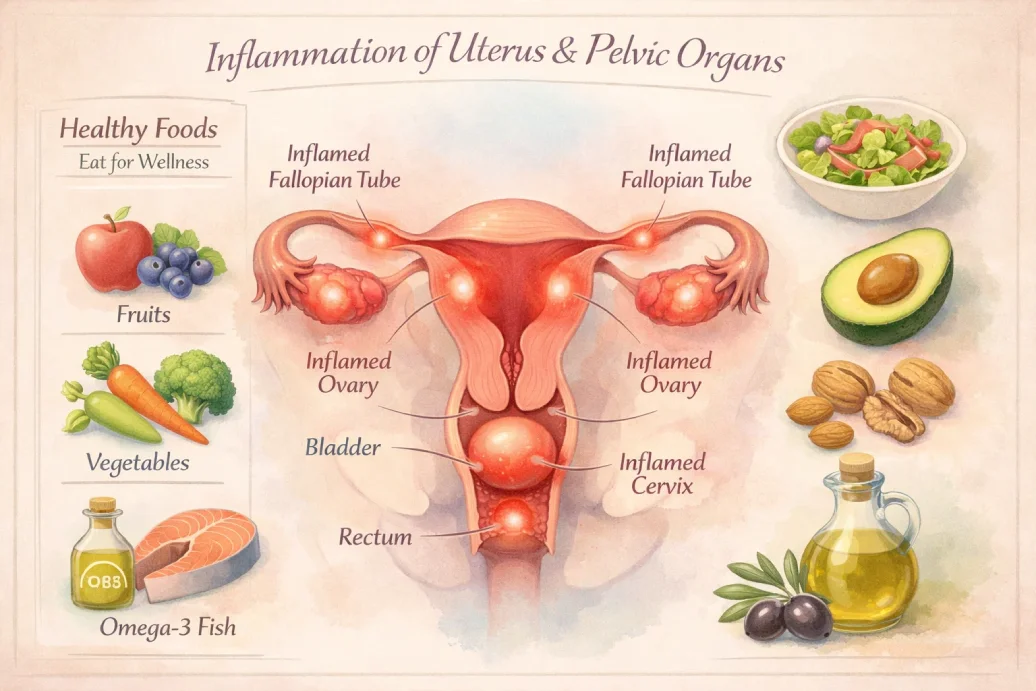
Studies show that chronic inflammation plays a major role in worsening endometriosis symptoms. Certain foods, especially those rich in trans fats and refined sugar, can elevate inflammatory markers like prostaglandins, aggravating pelvic pain. On the other hand, the endometriosis anti-inflammatory diet—which emphasizes whole grains, fruits, vegetables, lean proteins, and omega-3 fatty acids—helps calm systemic inflammation and improve gut health.
A nutritious diet also supports hormonal regulation by aiding the liver’s natural detoxification process. Fiber-rich foods assist in metabolizing excess estrogen, one of the hormones responsible for stimulating endometrial growth. Additionally, antioxidants from colorful plant-based foods protect cells from oxidative stress, a common issue in women with endometriosis.
At Mayflower Hospital, our specialists advocate a balanced, evidence-driven approach where endometriosis nutrition is personalized based on symptom severity, medical history, and lifestyle. This combination of medical expertise and dietary science helps women manage pain, improve digestion, and enhance reproductive well-being.
Next, we’ll explore specific food groups that research has identified as beneficial in easing symptoms—offering a clearer picture of what to eat when following an endometriosis-friendly diet.
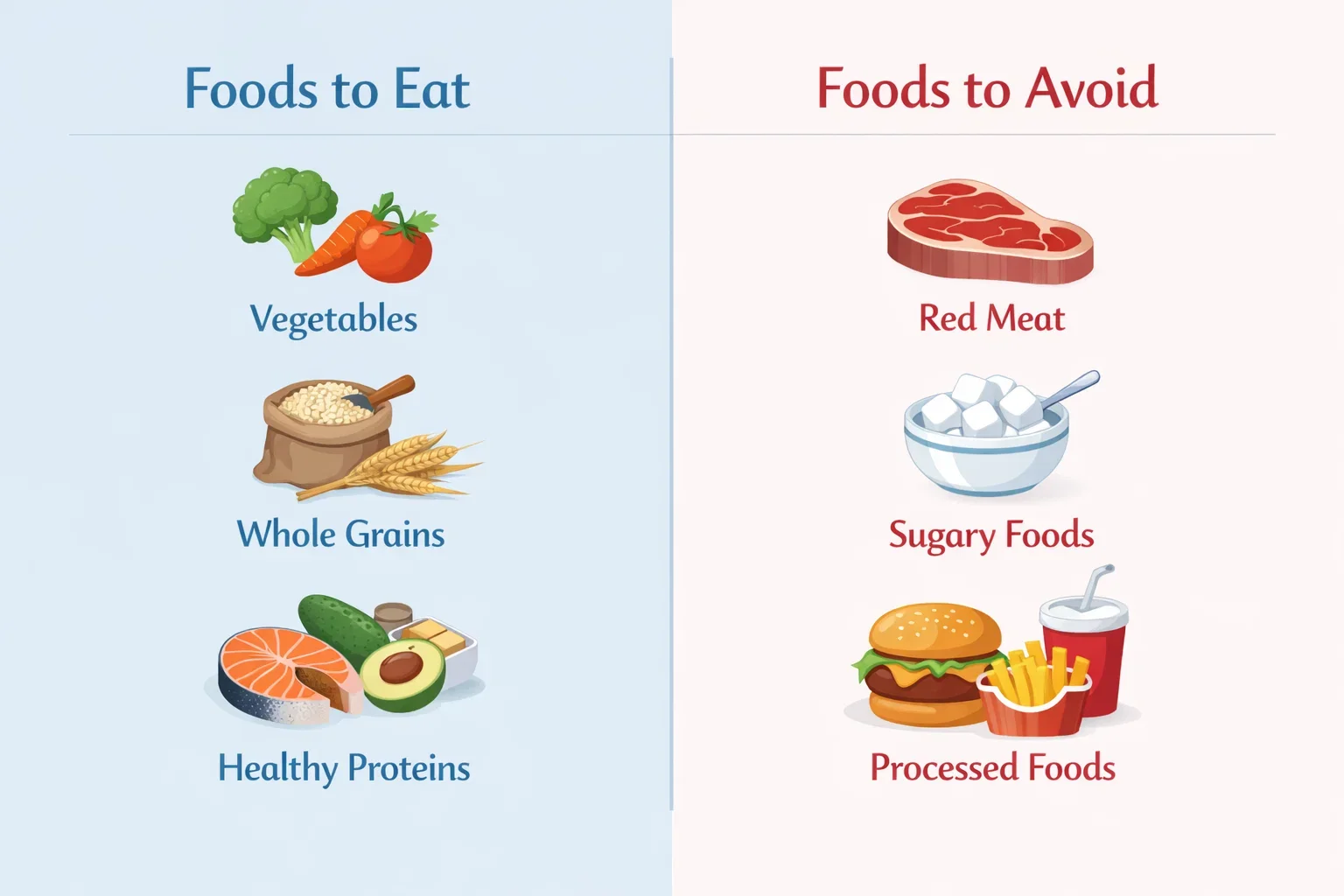
Foods to Eat for Endometriosis Relief
What you eat can either fuel inflammation or help your body fight it. Choosing the right foods is one of the most practical ways to manage symptoms naturally. A balanced, anti-inflammatory endometriosis diet focuses on nutrients that reduce pain, balance hormones, and support overall energy levels.
Below are research-supported food groups that form the foundation of a healthy diet for endometriosis.
Anti-Inflammatory Foods
Anti-inflammatory foods are at the core of every effective endometriosis diet plan. Omega-3 fatty acids found in salmon, chia seeds, flaxseeds, and walnuts are known to lower prostaglandin levels—compounds that cause cramping and pain. Similarly, brightly colored fruits and vegetables like berries, spinach, kale, and bell peppers contain antioxidants that neutralize free radicals and reduce oxidative stress within the pelvic region.
Turmeric and ginger are particularly powerful additions, thanks to their natural anti-inflammatory compounds, curcumin and gingerol. Incorporating these into soups, smoothies, or herbal teas can make daily symptom management easier.
Fiber-Rich Foods for Hormonal Balance
Fiber plays a crucial role in removing excess estrogen from the body, which can otherwise contribute to endometrial tissue growth. Whole grains like oats, brown rice, and quinoa, along with lentils, beans, and cruciferous vegetables such as broccoli and cauliflower, promote better hormone metabolism and gut health.
A high-fiber diet also supports weight management, improves digestion, and minimizes bloating—three common challenges for women dealing with endometriosis.

Plant-Based Proteins and Iron Sources
Plant-based proteins such as tofu, beans, lentils, and chickpeas are excellent options for those aiming to reduce red meat intake. They offer essential amino acids without triggering inflammatory pathways. Women with heavy menstrual bleeding due to endometriosis often experience iron deficiency, so including leafy greens, pumpkin seeds, and fortified cereals helps maintain healthy iron levels.
This approach is particularly beneficial for women managing endometriosis and PCOS, as both conditions respond positively to diets lower in saturated fats and higher in complex carbohydrates and micronutrients.
When planned correctly, these foods can help you feel fuller, more energized, and hormonally balanced—forming the foundation for long-term symptom relief. In the next section, we’ll look at foods you should limit or avoid to prevent inflammation from flaring up.
Foods to Avoid with Endometriosis
Just as some foods can soothe inflammation, others can trigger it. Understanding what to limit or eliminate is crucial to ensure your endometriosis diet works effectively. Research shows that certain foods increase estrogen levels, promote oxidative stress, or stimulate the production of inflammatory prostaglandins—all of which can worsen pelvic pain and fatigue.
Below are the main food categories experts recommend avoiding or minimizing in a diet for endometriosis.
Inflammatory Triggers
Processed and fried foods are among the top contributors to inflammation. Items like packaged snacks, fast food, and refined sugars release inflammatory molecules that aggravate pelvic pain. Red meat, especially when consumed frequently, can raise estrogen levels and prostaglandin production, intensifying menstrual cramps.
Opting for lean proteins or plant-based alternatives instead can make a noticeable difference in symptom severity and energy balance.
Gluten and Dairy Sensitivity
Many women report symptom improvement after reducing or eliminating gluten and dairy. A 2022 clinical study found that a gluten-free diet reduced pelvic pain in women with endometriosis by up to 75% over a 12-month period. Gluten and casein (the main protein in dairy) can trigger inflammatory responses in sensitive individuals, leading to bloating, fatigue, and increased inflammation.
If cutting them out entirely isn’t practical, consider limiting intake and observing how your body responds.
Caffeine and Alcohol Effects
Both caffeine and alcohol can disrupt hormone metabolism and increase estrogen levels. While moderate coffee or tea intake may not cause issues for everyone, excessive caffeine can worsen anxiety, sleep issues, and inflammation. Alcohol, especially red wine and spirits, may impair liver function—the organ responsible for metabolizing excess estrogen.
Replacing these with herbal teas and anti-inflammatory beverages like turmeric milk or green tea can help maintain hormonal balance.
When you remove inflammatory foods, your body responds better to nutritional therapy and medical treatment. The next section explains how to build a practical, research-backed endometriosis diet plan tailored to your needs.
Building a Research-Backed Endometriosis Diet Plan
An effective endometriosis diet plan combines scientific evidence with everyday practicality. It’s not about strict restriction, but about creating a balanced and sustainable eating pattern that reduces inflammation, supports hormonal balance, and maintains energy levels throughout the day.
At Mayflower Hospital, our nutrition experts design meal plans personalized to your lifestyle, symptom pattern, and treatment goals. Below is a simple, research-backed outline to help you get started.
Sample Daily Meal Plan
A balanced day on an endometriosis anti-inflammatory diet might look like this:
Breakfast:
Oatmeal topped with flaxseeds, blueberries, and almond milk — rich in fiber and antioxidants for hormonal balance.
Mid-Morning Snack:
A handful of walnuts or roasted chickpeas to stabilize blood sugar.
Lunch:
Quinoa salad with spinach, grilled tofu, and olive oil dressing. Add turmeric and lemon juice for anti-inflammatory benefits.
Evening Snack:
Green tea with a slice of avocado toast or fruit.
Dinner:
Steamed vegetables, brown rice, and baked salmon or lentil stew.
Hydration Tip:
Drink at least 2 liters of water daily and include herbal teas like ginger or chamomile to aid digestion and reduce bloating.
This structure can be modified to suit vegetarian, vegan, or gluten-free preferences.
Endometriosis Diet Recipes
Simple, home-friendly endometriosis diet recipes can make nutrition enjoyable:
- Anti-inflammatory smoothie: Blend spinach, banana, turmeric, flaxseeds, and almond milk.
- Omega-rich salad bowl: Combine leafy greens, chickpeas, olive oil, and sunflower seeds.
- Warm turmeric soup: Carrot, ginger, and turmeric with a drizzle of olive oil — comforting and anti-inflammatory.
Each of these recipes provides fiber, healthy fats, and antioxidants to naturally calm inflammation.
Endometriosis Diet Grocery List
Stocking your kitchen with the right items makes adherence easier.
Pantry staples: Oats, brown rice, quinoa, lentils, chickpeas, olive oil, turmeric powder.
Fresh produce: Spinach, broccoli, berries, citrus fruits, sweet potatoes.
Proteins: Tofu, beans, nuts, seeds, and fish (if non-vegetarian).
Beverages: Herbal teas, almond milk, coconut water.
For convenience, Mayflower’s nutrition team provides patients with tailored endometriosis diet grocery lists that match their calorie needs and treatment plans.
A well-prepared grocery list ensures you always have anti-inflammatory foods within reach, helping you stay consistent with your dietary goals. In the next section, we’ll explore the latest global research that supports these dietary recommendations.

What Latest Research Says About Nutrition and Endometriosis
Scientific research over the past decade has significantly strengthened the connection between nutrition and endometriosis. Emerging evidence suggests that diet can influence not just inflammation but also hormonal regulation, oxidative stress, and immune function — all key factors in managing endometriosis progression and symptoms.
A 2023 PubMed review found that women following a Mediterranean-style diet — rich in olive oil, vegetables, legumes, whole grains, and fish — experienced a noticeable reduction in pelvic pain and fatigue within 12 weeks. The study linked this improvement to higher intake of omega-3 fatty acids and antioxidants, which help inhibit prostaglandin production and reduce inflammation in endometrial tissue.
Similarly, researchers from the National Institutes of Health (NIH) have highlighted the role of vitamin D, zinc, and selenium in regulating immune response and supporting hormonal balance in women with endometriosis. These micronutrients may help suppress abnormal tissue growth and oxidative stress at the cellular level.
Other studies support the benefits of low-FODMAP and gluten-free diets, particularly for those with gastrointestinal discomfort or co-existing irritable bowel syndrome (IBS). These dietary approaches promote gut healing, enhance nutrient absorption, and reduce systemic inflammation.
While there is no single “cure diet,” the consensus among medical experts is clear: incorporating whole, anti-inflammatory, and nutrient-dense foods improves overall quality of life for those managing endometriosis.
At Mayflower Women’s Hospital, we integrate these global research findings into customized care plans, combining clinical expertise with nutritional therapy to support sustainable, science-backed results.
The next section explains how this research-driven dietary care integrates seamlessly with medical treatment to create a holistic healing experience.
Combining Medical and Nutritional Care
While following an endometriosis diet helps control symptoms, long-term relief often requires an integrated approach combining medical expertise and personalized nutrition. At Mayflower Women’s Hospital, this philosophy forms the foundation of patient care—where gynecologists, laparoscopic surgeons, and nutrition specialists collaborate to deliver comprehensive treatment.
Dietary therapy complements medical interventions such as hormonal regulation, pain management, and minimally invasive surgeries. By reducing inflammation and improving hormonal metabolism, an evidence-based endometriosis nutrition plan enhances the effectiveness of these medical treatments. Patients who maintain balanced eating habits often experience shorter recovery times, better digestion, and improved overall energy levels.
Our experts also emphasize sustainable lifestyle changes. Beyond diet, factors like sleep, hydration, exercise, and stress management contribute significantly to symptom control. The goal is not merely symptom suppression but long-term hormonal and metabolic balance—helping patients reclaim their everyday comfort and confidence.
If you’re undergoing medical or surgical care for endometriosis, consult our team to create a personalized diet plan that aligns with your treatment. A multidisciplinary approach ensures that every aspect of your well-being—nutritional, physical, and emotional—is supported through each phase of recovery.
Conclusion
Adopting a research-backed endometriosis diet is one of the most effective ways to complement medical treatment and improve daily well-being. By emphasizing anti-inflammatory foods, balanced nutrients, and mindful eating, women can manage pain, reduce fatigue, and support long-term hormonal stability.
At Mayflower Women’s Hospital, we believe in evidence-based, compassionate care that integrates nutrition with modern gynecological expertise. Our team of gynecologists, laparoscopic surgeons, and dietitians collaborate to provide personalized solutions for every patient—helping you feel healthier, stronger, and more in control of your body.
If you’re looking for an individualized endometriosis diet plan or medical management guidance, consult our specialists today and take a step toward a healthier, pain-free future.
Frequently Asked Questions
The best diet for endometriosis emphasizes anti-inflammatory, plant-based foods such as leafy greens, fruits, whole grains, and omega-3-rich sources like salmon and walnuts. A Mediterranean-style plan helps regulate hormones, reduce pain, and improve gut health.
Avoid processed foods, red meat, refined sugars, excessive caffeine, and alcohol. These can raise inflammation and estrogen levels, worsening symptoms. Gluten and dairy may also trigger discomfort in some women; consider a short-term elimination approach under guidance.
Yes. Research shows that following an endometriosis anti-inflammatory diet can lower prostaglandin production—chemicals responsible for menstrual pain. Omega-3s, turmeric, and antioxidants from fruits and vegetables play a major role in pain reduction.
A nutrient-rich, low-sugar diet supports both endometriosis and PCOS by improving insulin sensitivity and balancing hormones. Foods high in fiber, lean protein, and healthy fats aid in regulating menstrual cycles and reducing inflammation.
Maintaining a balanced diet low in sodium and rich in fruits, vegetables, and whole grains helps reduce risk. Regular prenatal check-ups and hydration are equally important. (Internal Linking Idea: For more insights, read our guide on Gestational Hypertension: Risks and Management)
Author
-

Dr. Smeet, true to his name, is known for his warm personality and cheerful smile that make patients instantly feel at ease with him.
Until now, he has performed 8000+ surgeries and several of which are supra-major surgeries for deep infiltrating endometriosis and fertility enhancing surgeries. With several publications in notable journals, he is constantly pushing the envelope of possibilities in gynecological surgeries