Endometriosis infertility is one of the most challenging reproductive health issues many women face. Endometriosis, a condition where tissue similar to the uterine lining grows outside the uterus, can significantly affect a woman’s ability to conceive. While not every woman with endometriosis will develop infertility, research shows that up to 30–50% of women with this condition may struggle with conception. For women trying to start or expand their families, understanding this link is essential.
This blog explains how endometriosis causes infertility, the treatment options available, the role of IVF and surgery, lifestyle changes that can help, and real success stories that offer hope.
Understanding Endometriosis and Infertility
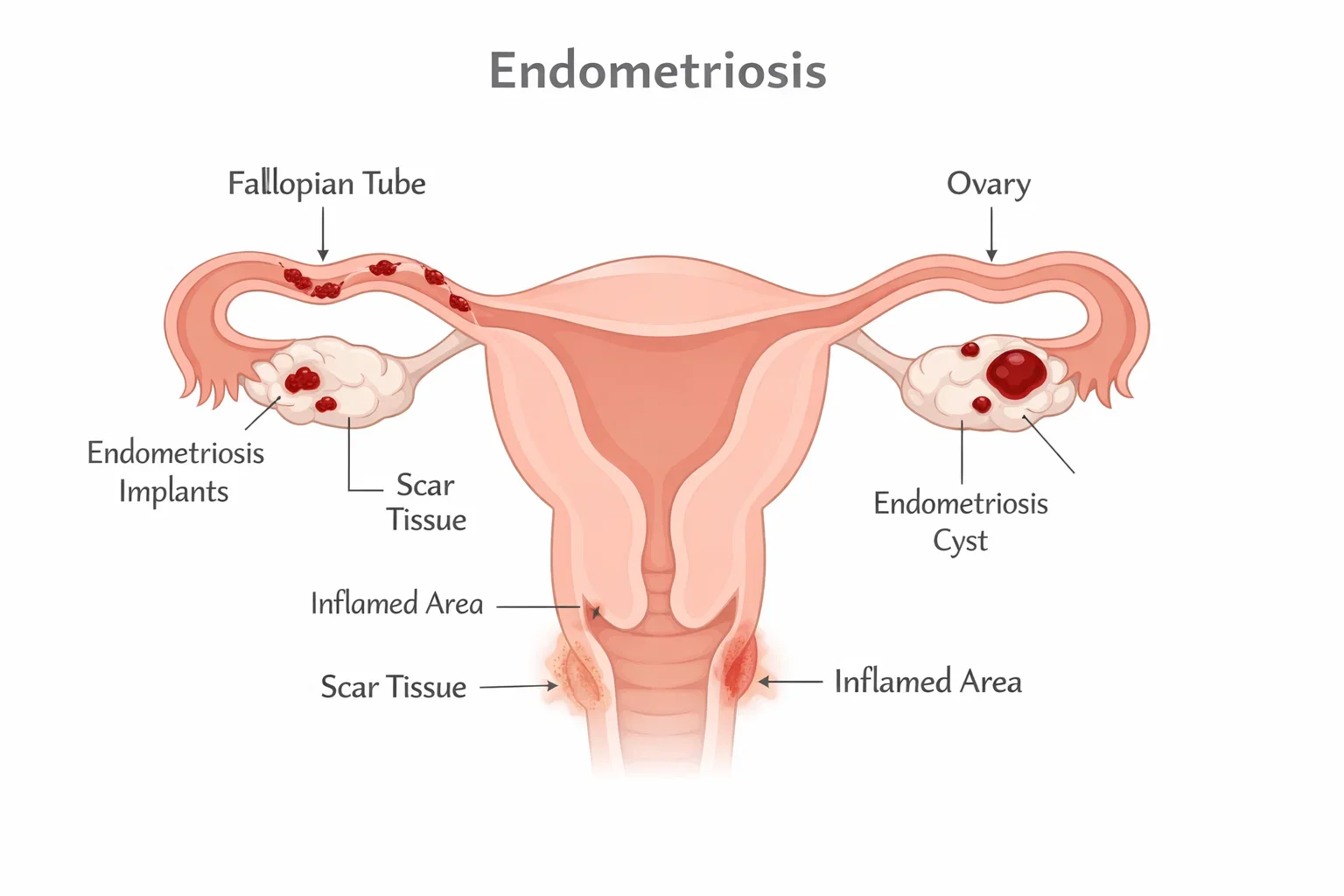
Endometriosis is a chronic gynecological condition where endometrial-like tissue grows on structures such as the ovaries, fallopian tubes, pelvic lining, and sometimes even beyond the reproductive organs. These misplaced tissue deposits can thicken, break down, and bleed with each menstrual cycle, causing inflammation, scarring, and adhesions.
But does endometriosis cause infertility? The answer is not always straightforward. Some women with endometriosis conceive naturally, while others face significant obstacles. The condition’s effect on fertility depends on factors such as disease stage, location of lesions, and presence of scar tissue.
How Does Endometriosis Cause Infertility?
- Blocked fallopian tubes: Adhesions may distort reproductive anatomy, preventing egg and sperm from meeting.
- Poor egg quality: Chronic inflammation can affect ovarian reserve and egg development.
- Hormonal imbalance: Endometriosis may disrupt ovulation.
- Inflammatory environment: Excessive pelvic inflammation can reduce embryo implantation chances.
The infertility impact varies – while mild endometriosis may not prevent conception, advanced stages often reduce natural fertility rates significantly.
How Common is Infertility in Endometriosis?
Endometriosis is one of the leading causes of infertility worldwide. Studies suggest that 30–50% of women with endometriosis experience fertility challenges, compared to 10–20% in the general population. This means women with the condition are two to three times more likely to face difficulties when trying to conceive.
The prevalence is also tied to the stage of endometriosis. Doctors classify the disease into four stages based on severity:
Stage-Wise Infertility Risk
- Stage 1 (Minimal) – Small lesions, minimal scarring. Fertility is often unaffected, and many women can conceive naturally.
- Stage 2 (Mild) – More lesions with some adhesions. Fertility challenges may start to appear but natural conception is still possible.
- Stage 3 (Moderate) – Endometriomas (ovarian cysts) and more adhesions are common. Natural conception rates drop, and assisted reproductive techniques may be needed.
- Stage 4 (Severe) – Large cysts, extensive adhesions, and pelvic anatomy distortion. Natural conception is rare, and most women require fertility treatments like IVF.
For women with stage 4 endometriosis infertility, reproductive specialists often recommend a combination of surgery and assisted reproduction for the best outcomes.
Endometriosis infertility rate varies widely because each woman’s reproductive health is unique. Factors such as age, ovarian reserve, presence of other conditions (like fibroids or PCOS), and overall lifestyle also play a role in determining fertility chances.
Symptoms That May Indicate Endometriosis-Related Infertility
One of the challenges with endometriosis infertility is that symptoms may overlap with general gynecological issues. Many women don’t realize they have endometriosis until they face difficulties while trying to conceive. Recognizing the early signs can help in timely diagnosis and intervention.
Common Symptoms Linked to Infertility
- Painful periods (dysmenorrhea): Severe cramps before and during menstruation.
- Chronic pelvic pain: Ongoing discomfort in the lower abdomen or pelvis.
- Pain during intercourse (dyspareunia): A frequent sign of advanced endometriosis.
- Heavy menstrual bleeding: May signal deeper tissue involvement.
- Painful bowel movements or urination during periods: Suggests lesions beyond the uterus.
Signs While Trying to Conceive
Many women only discover their condition when they experience difficulty conceiving. Some of the warning indicators include:
- Longer time to get pregnant: Even after a year of unprotected intercourse.
- Repeated early miscarriages: Possibly linked to inflammation and poor implantation.
- Irregular menstrual cycles: Hormonal imbalance caused by endometriosis can disrupt ovulation.
For women who are actively trying to conceive with endometriosis, these symptoms are strong cues to consult our fertility specialist. Prompt evaluation improves the chances of effective treatment and successful pregnancy outcomes.
How Endometriosis is Diagnosed in Infertility Cases
For women struggling with endometriosis infertility, early and accurate diagnosis is essential. Since the condition can mimic other pelvic disorders, doctors use a combination of medical history, imaging, and surgical evaluation to confirm endometriosis and its impact on fertility.

Medical History and Symptom Review
A gynecologist begins by assessing symptoms such as painful periods, pelvic pain, and difficulty conceiving. A detailed reproductive history -including previous pregnancies, miscarriages, or infertility duration -helps guide further tests.
Imaging Techniques
- Ultrasound: Can detect ovarian endometriomas (cysts), but may miss smaller lesions.
- MRI (Magnetic Resonance Imaging): Provides a detailed view of pelvic structures, useful for mapping deep infiltrating endometriosis.
Laparoscopy – The Gold Standard
Laparoscopy is a minimally invasive surgical procedure where a small camera is inserted into the abdomen. It allows doctors to:
- Directly visualize endometriosis lesions.
- Assess scarring, adhesions, and blocked fallopian tubes.
- Remove or treat endometriosis deposits during the same procedure.
This dual diagnostic and therapeutic approach makes laparoscopy the most reliable method for evaluating endometriosis-related infertility.
Timely diagnosis ensures that patients receive tailored treatment strategies -from medication to surgery to assisted reproductive options -improving their chances of conceiving successfully.
Endometriosis Infertility Treatment Options
Treating endometriosis infertility often requires a multi-layered approach. The right strategy depends on factors such as age, disease stage, ovarian reserve, and how long the couple has been trying to conceive. Treatments may include lifestyle changes, surgery, medications, or advanced fertility techniques.
Lifestyle and Conservative Care
- Healthy weight management: Obesity can worsen inflammation and disrupt ovulation.
- Balanced fertility diet: Anti-inflammatory foods like leafy greens, salmon, nuts, and whole grains support reproductive health.
- Supplements: Omega-3 fatty acids, vitamin D, and antioxidants may improve egg quality.
- Pain management: NSAIDs or physiotherapy help relieve symptoms but do not directly restore fertility.
Surgical Approaches
Endometriosis fertility surgery is often recommended when lesions or adhesions are preventing conception.
- Laparoscopic excision or ablation: Removes or destroys visible endometriosis tissue.
- Adhesiolysis: Frees blocked fallopian tubes or ovaries stuck by scar tissue.
- Ovarian cyst removal: Improves ovarian function but must be balanced against the risk of reducing egg reserve.

Surgery can improve natural conception rates, especially in stage 3–4 cases, and may enhance the success of subsequent IVF.
Medical Therapy
Hormonal treatments (oral contraceptives, GnRH agonists) are effective in controlling symptoms but usually suppress ovulation, making them unsuitable while trying to conceive. They are more useful in managing symptoms between fertility treatments.
In summary, a customized plan that combines surgery, lifestyle adjustments, and fertility assistance provides the best chance for overcoming endometriosis-related infertility.
Assisted Reproductive Techniques (ART) and Endometriosis
When natural conception is difficult, fertility specialists often recommend assisted reproductive techniques. For women facing endometriosis infertility, ART such as IUI and IVF can significantly improve pregnancy chances, especially when surgery alone is not enough.
Intrauterine Insemination (IUI) for Mild to Moderate Endometriosis
IUI may be considered for women with:
- Minimal to mild endometriosis (Stage 1–2).
- Normal ovarian reserve and open fallopian tubes.
- No severe adhesions or endometriomas.
Although IUI success rates in endometriosis patients are slightly lower compared to unexplained infertility, it remains a cost-effective first step before advanced ART.
In Vitro Fertilization (IVF) for Advanced Endometriosis
For stage 3 and stage 4 endometriosis infertility, IVF is often the most effective option.
- Eggs are retrieved directly from the ovaries and fertilized in a lab.
- Embryos are then transferred to the uterus, bypassing blocked or damaged tubes.
- This process eliminates many physical barriers caused by scarring and adhesions.
Endometriosis IVF success rate varies depending on the stage and patient’s age. Studies show:
- Stage 1–2: Similar outcomes to women without endometriosis.
- Stage 3–4: Lower success rates, but still much higher than trying naturally.
- Post-surgery IVF: Outcomes often improve compared to untreated cases.
Advanced ART Options
- Intracytoplasmic Sperm Injection (ICSI): A single sperm is injected into an egg, often used when egg quality is affected.
- Frozen embryo transfer (FET): May enhance implantation rates by allowing the uterus to recover from stimulation cycles.
- Egg or embryo freezing: Helpful for women delaying pregnancy after endometriosis surgery.
For many couples, combining surgery with ART provides the best pathway to overcome endometriosis infertility and achieve pregnancy.
Stage-Wise Fertility Outcomes in Endometriosis
The effect of endometriosis on fertility varies significantly depending on the stage of the disease. The American Society for Reproductive Medicine (ASRM) classifies endometriosis into four stages -from minimal to severe -based on the size, depth, and spread of lesions, as well as the degree of adhesions.
Stage 1–2 (Minimal to Mild Endometriosis)
- Fertility impact is relatively low.
- Natural conception is still possible for many women.
- Studies show pregnancy rates close to those of women without endometriosis.
- If conception does not occur within 6–12 months, treatments such as IUI or surgery may be recommended.
Stage 3–4 (Moderate to Severe Endometriosis)
- Adhesions, ovarian cysts (endometriomas), and distorted pelvic anatomy reduce fertility.
- Stage 4 endometriosis infertility often requires IVF or surgical intervention.
- Success rates are lower compared to earlier stages but can improve significantly with surgery followed by ART.
Key Considerations Across Stages
- Age factor: Women over 35 face additional challenges regardless of stage.
- Ovarian reserve: Severe cases may reduce egg count and quality.
- Surgery + ART: Often recommended for moderate and severe cases to maximize pregnancy chances.
Overall, while endometriosis infertility is more likely in advanced stages, personalized treatment plans can still lead to successful conception.
Lifestyle and Emotional Support in Endometriosis Infertility
Managing endometriosis infertility is not only about medical treatments. Lifestyle habits, diet, and emotional wellbeing play a vital role in improving fertility potential and supporting women through their journey.
Fertility-Friendly Diet and Lifestyle Choices
Research suggests that adopting an endometriosis fertility diet can improve egg quality, reduce inflammation, and balance hormones. Some effective changes include:
- Anti-inflammatory foods: Leafy greens, berries, tomatoes, and olive oil.
- Omega-3 rich proteins: Salmon, walnuts, chia seeds.
- Antioxidants: Vitamin C and E-rich fruits help combat oxidative stress on eggs.
- Limiting red meat and processed foods: Reduces estrogen dominance and inflammation.
Regular physical activity such as yoga, Pilates, or low-impact aerobics improves blood circulation, reduces stress, and may alleviate pelvic discomfort.
Stress Management and Mind-Body Practices
Infertility can create a cycle of anxiety and stress, which may further affect reproductive hormones. Helpful practices include:
- Mindfulness and meditation: Reduce cortisol levels and improve emotional stability.
- Acupuncture: Some studies suggest it may boost blood flow to the uterus and enhance IVF success rates.
- Sleep hygiene: Consistent, quality sleep supports hormone balance.
Emotional and Psychological Support
The emotional toll of infertility is often underestimated. Couples facing endometriosis-related infertility may experience frustration, isolation, and loss of confidence.
- Counseling and therapy provide coping strategies.
- Support groups connect women with similar experiences.
- Positive success stories inspire hope and reduce feelings of helplessness.
Caring for both body and mind ensures women are better prepared for fertility treatments and more resilient throughout the journey.
Real-Life Success Stories: Hope After Endometriosis Infertility
Hearing about other women’s journeys can inspire hope and reassure those facing endometriosis infertility that pregnancy is still possible with the right care.
Natural Conception After Treatment
Some women with mild to moderate endometriosis conceive naturally after laparoscopic surgery. By removing adhesions and restoring pelvic anatomy, fertility can be significantly improved. Many patients report conceiving within a year following surgery.
IVF Success After Endometriosis
For women with stage 4 endometriosis infertility, IVF often provides the best path to pregnancy. At Mayflower Hospital, patients who had previously tried unsuccessfully for years achieved success after undergoing IVF combined with advanced techniques such as ICSI and frozen embryo transfer. These cases highlight that, despite lower average rates, endometriosis IVF success rate can be favorable with expert management.
Pregnancy After Endometriosis Surgery

Several women who underwent endometriosis fertility surgery later conceived, both naturally and with ART support. Surgery helps reduce pain, restore anatomy, and prepare the reproductive system for successful implantation. For many, this was the turning point in their journey.
These endometriosis infertility success stories show that while the journey may be difficult, the outcome is often rewarding. With medical support, lifestyle changes, and emotional resilience, women can overcome infertility challenges and achieve their dream of parenthood.
When to Seek Medical Help
While some women with endometriosis infertility may conceive naturally, knowing when to seek professional help is crucial. Early intervention can prevent years of uncertainty and improve success rates with treatment.
How Long Should You Try Before Consulting a Specialist?
- Women under 35: Seek help if pregnancy does not occur after 12 months of regular, unprotected intercourse.
- Women over 35: Consult a fertility specialist after 6 months of trying.
- Immediate evaluation: Recommended for women with known endometriosis, severe pelvic pain, or irregular cycles.
Red Flags That Need Prompt Attention
- Intense menstrual cramps or chronic pelvic pain.
- Repeated miscarriages.
- Evidence of blocked fallopian tubes or ovarian cysts.
- Stage 3–4 diagnosis of endometriosis.
Expert Care at Mayflower Hospital
At Mayflower Hospital, our fertility specialists combine advanced diagnostic tools, minimally invasive endometriosis surgery, and state-of-the-art IVF technologies to help women achieve pregnancy. Each treatment plan is customized, ensuring patients receive the best chance at conception while managing endometriosis symptoms effectively.
If you are struggling to conceive and suspect endometriosis may be a factor, timely medical guidance can make all the difference.
Preventive and Long-Term Management
While there is no permanent cure for endometriosis, proactive management can improve fertility outcomes and reduce recurrence after treatment. For women dealing with endometriosis infertility, focusing on long-term health ensures better chances of conception in the future.
Regular Monitoring After Surgery
Even after endometriosis fertility surgery, lesions can return. Regular check-ups and imaging help detect recurrence early, allowing timely treatment before it impacts fertility again.
Lifestyle Modifications
- Balanced diet: Continuing an anti-inflammatory diet reduces flare-ups and supports hormonal balance.
- Exercise: Regular activity maintains healthy weight, improves circulation, and lowers stress.
- Limiting toxins: Reducing alcohol, caffeine, and smoking helps protect reproductive health.
Medical Support Between Treatments
- Hormonal therapy: May be prescribed post-surgery to suppress regrowth when pregnancy is not immediately planned.
- Supplements: Vitamins and minerals to support ovarian health.
- Holistic therapies: Stress management, yoga, or acupuncture to maintain wellness.
Balancing Fertility Goals with Long-Term Health
Not every woman wants to pursue pregnancy immediately. For those delaying conception, options such as egg or embryo freezing allow preservation of fertility potential. Long-term planning helps women align their reproductive goals with lifestyle and health priorities.
By combining medical care, preventive strategies, and consistent monitoring, women can manage endometriosis more effectively while safeguarding their fertility.
Conclusion
Endometriosis infertility can feel overwhelming, but it is not the end of the journey toward parenthood. While endometriosis can interfere with fertility through inflammation, scarring, and hormonal imbalance, a combination of treatments -from surgery to ART like IVF -has helped countless women conceive successfully.
With proper diagnosis, personalized treatment, lifestyle changes, and emotional support, women can significantly improve their chances of pregnancy. At Mayflower Hospital, our specialists provide evidence-based care, guiding women through each stage of treatment with compassion and expertise.
Every woman’s fertility journey is unique – and with the right medical and emotional support, pregnancy is possible, even after advanced endometriosis.
FAQ
No. Not all women with endometriosis will experience infertility. While up to 50% may face difficulties, many still conceive naturally, especially in the early stages.
Natural pregnancy is rare in stage 4 cases due to extensive adhesions and cysts, but it is still possible for some. Most women benefit from surgery or IVF.
Endometriosis IVF success rate varies by stage and age. In mild cases, success rates are similar to women without endometriosis, while advanced cases may have slightly lower outcomes.
Endometriosis fertility surgery removes adhesions, cysts, and lesions, restoring pelvic anatomy and improving natural conception chances or enhancing IVF outcomes.
Following an endometriosis fertility diet, exercising regularly, managing stress, and avoiding smoking or excessive alcohol can all support reproductive health.
Yes, many women conceive and carry healthy pregnancies after surgery. Regular follow-up with a gynecologist ensures ongoing safety and monitoring.
Author
-

Dr. Smeet, true to his name, is known for his warm personality and cheerful smile that make patients instantly feel at ease with him.
Until now, he has performed 8000+ surgeries and several of which are supra-major surgeries for deep infiltrating endometriosis and fertility enhancing surgeries. With several publications in notable journals, he is constantly pushing the envelope of possibilities in gynecological surgeries