Endometriosis MRI plays a vital role in accurately detecting one of the most complex conditions affecting women’s reproductive health. Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, leading to chronic pain, inflammation, and fertility challenges. Despite being common, it often goes undiagnosed for years due to the limitations of traditional tests and the variability of symptoms.
With advancements in diagnostic imaging, MRI for endometriosis diagnosis has become a non-invasive, high-precision tool that helps visualize deep pelvic lesions, adhesions, and organ involvement in detail. However, the true power of MRI lies not only in technology but in professional MRI reading – interpreting subtle findings accurately to distinguish between different forms and stages of endometriosis.
At Mayflower Women’s Hospital, our team of Endometriosis MRI specialists uses advanced pelvic MRI systems designed for women’s health. Their expert interpretation ensures early and precise detection, supporting more effective treatment planning and improved patient outcomes. Accurate imaging means reduced diagnostic delays and a better quality of life for women experiencing pelvic pain or infertility linked to endometriosis.
Understanding Endometriosis and Its Diagnostic Challenges
What Is Endometriosis?
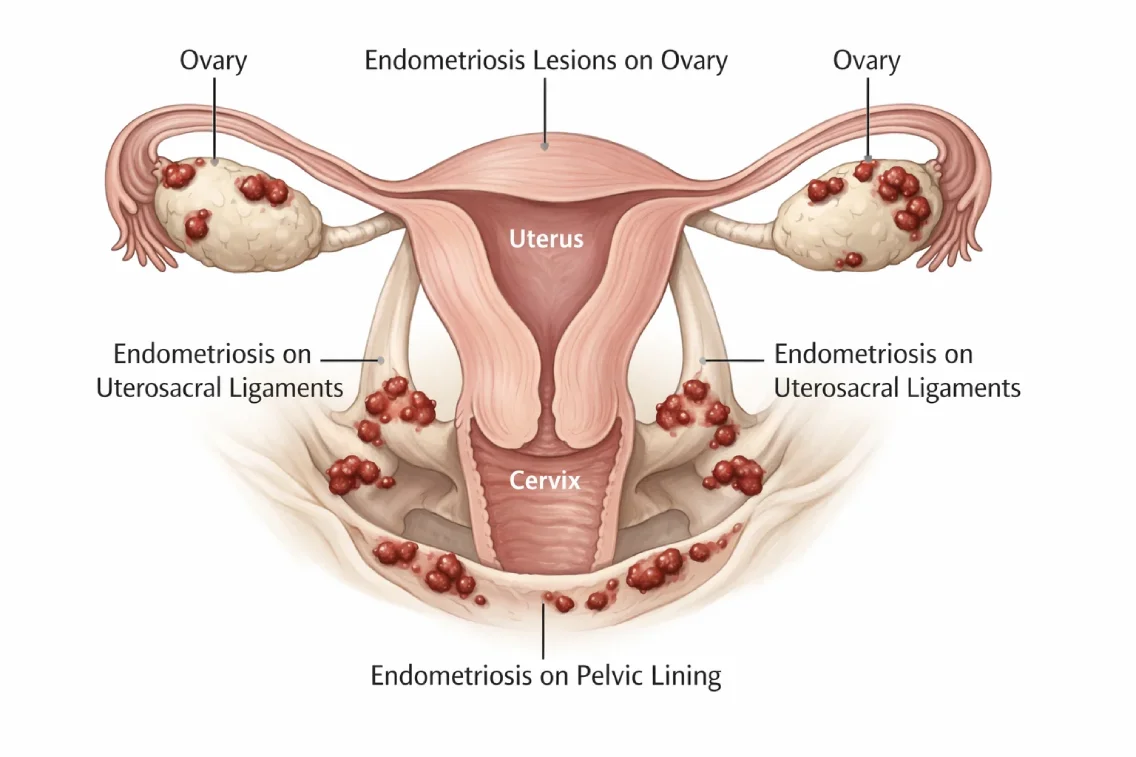
Endometriosis is a chronic condition where tissue similar to the endometrium – the lining of the uterus – grows outside the uterus, often affecting the ovaries, fallopian tubes, and pelvic lining. These growths respond to hormonal changes during the menstrual cycle, leading to inflammation, scarring, and chronic pain. Women with endometriosis may experience painful periods, pelvic discomfort, bloating, painful intercourse, and, in many cases, infertility.
Despite its prevalence, diagnosing endometriosis remains challenging because symptoms vary greatly and often resemble other disorders such as irritable bowel syndrome or pelvic inflammatory disease. This overlap makes it difficult to identify the condition based solely on symptoms or physical examinations.
Why Accurate Diagnosis Is Often Delayed
Many women wait years before receiving a correct diagnosis. Studies show that the average delay between symptom onset and diagnosis can range from 7 to 10 years. Traditional diagnostic methods, such as pelvic ultrasound or exploratory laparoscopy, may fail to detect deep or microscopic lesions.
The limitations of conventional imaging highlight the need for advanced, non-invasive endometriosis diagnosis methods like MRI. With high-resolution pelvic imaging, doctors can visualize the location and extent of endometrial tissue, ensuring timely and precise treatment.
For comprehensive care, Mayflower Women’s Hospital integrates gynecological expertise with advanced imaging facilities, allowing a coordinated approach to accurate detection and long-term management.
How Is Endometriosis Diagnosed Today? (Step-by-Step Clinical Pathway)
The Modern Diagnostic Approach
Accurately identifying endometriosis involves a combination of clinical evaluation, imaging, and, in certain cases, minimally invasive procedures. The diagnostic journey typically begins when a woman reports chronic pelvic pain, painful periods, or fertility issues. Gynecologists assess medical history, perform a pelvic examination, and may recommend imaging to confirm or rule out endometriosis.
In today’s medical practice, clinicians rely on structured diagnostic steps that progress from non-invasive to confirmatory methods. This sequence minimizes patient discomfort while improving diagnostic precision.
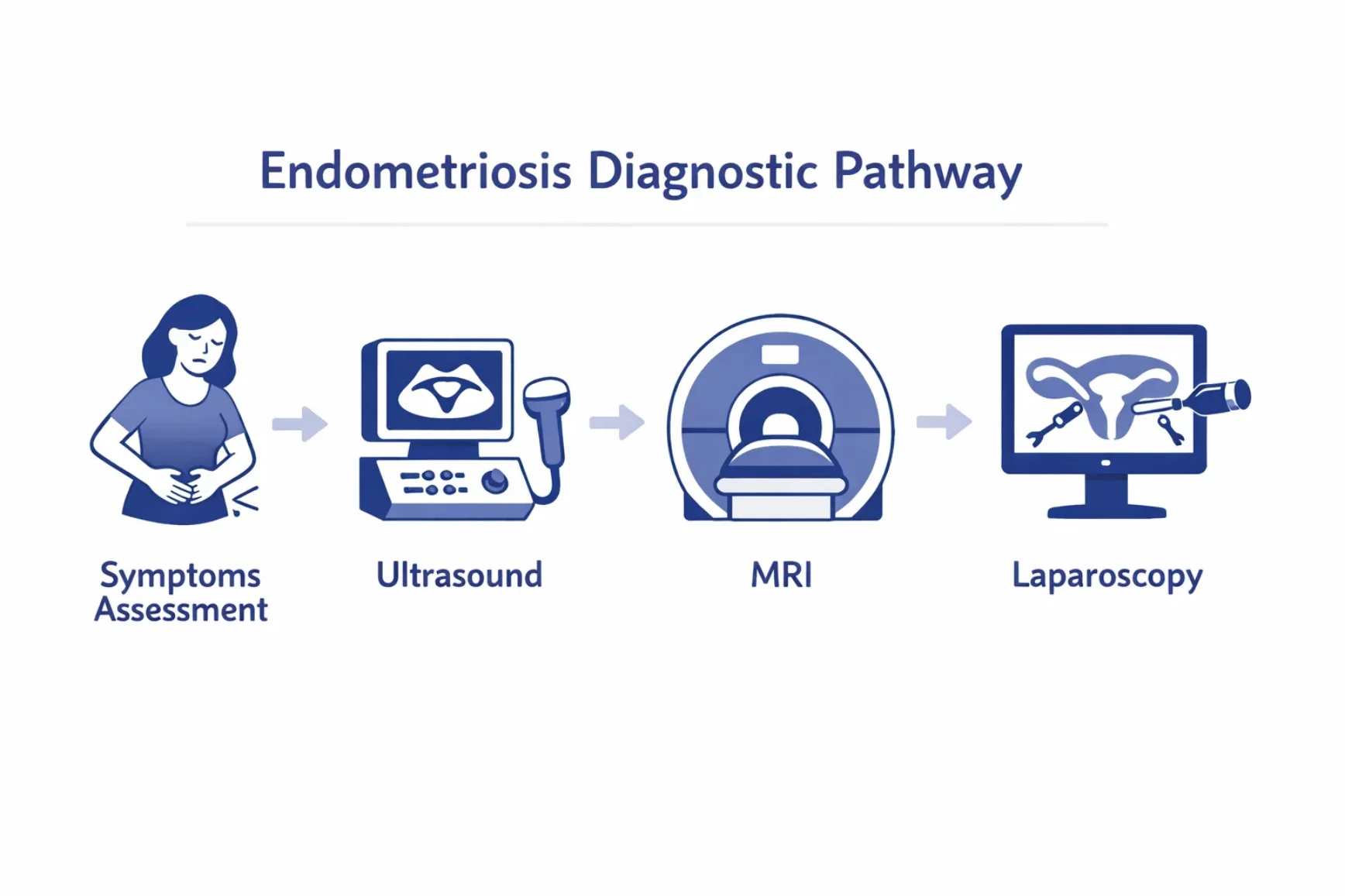
Step 1 – Clinical Evaluation and Symptom Mapping
Doctors begin by understanding the patient’s symptoms, menstrual patterns, and pain intensity. Endometriosis often presents differently in each woman, making personalized evaluation essential. Symptom mapping – where pain locations are correlated with possible lesion sites – guides further testing.
Step 2 – Ultrasound as the First Imaging Tool
Ultrasound is the initial imaging test for suspected endometriosis due to its accessibility and cost-effectiveness. However, it has limitations in detecting deep or hidden lesions. Endometriosis ultrasound can identify ovarian cysts (endometriomas) but may miss adhesions or peritoneal involvement.
This is why specialists often use ultrasound results as a preliminary screening before moving to more detailed imaging such as MRI.
Step 3 – MRI for Endometriosis Diagnosis
The MRI scan for endometriosis offers a detailed, high-resolution view of pelvic anatomy, making it the most advanced imaging method for non-invasive diagnosis. It helps visualize:
- Deep infiltrating endometriosis (DIE)
- Adhesions and organ displacement
- Lesions near the bowel, bladder, or uterosacral ligaments
When performed and interpreted by an Endometriosis MRI specialist, MRI can pinpoint the exact size and spread of lesions, allowing doctors to plan treatment without exploratory surgery.
Step 4 – Laparoscopy for Confirmation (If Needed)
While MRI provides strong diagnostic accuracy, laparoscopy remains the gold standard for confirmation in select cases. It involves inserting a camera through a small incision to directly view and, if necessary, remove lesions. However, with the rising precision of MRI imaging, many patients can now avoid this invasive procedure altogether.
Integrating Non-Invasive Diagnosis at Mayflower Hospital
At Mayflower Women’s Hospital, our multidisciplinary diagnostic protocol combines clinical expertise, ultrasound, and MRI to ensure accurate identification. By focusing on non-invasive endometriosis diagnosis, we minimize surgical interventions and provide faster, evidence-based results – empowering women to begin treatment without unnecessary delays.
Can MRI Detect Endometriosis? (A Scientific Overview)
Understanding the Role of MRI in Endometriosis Detection
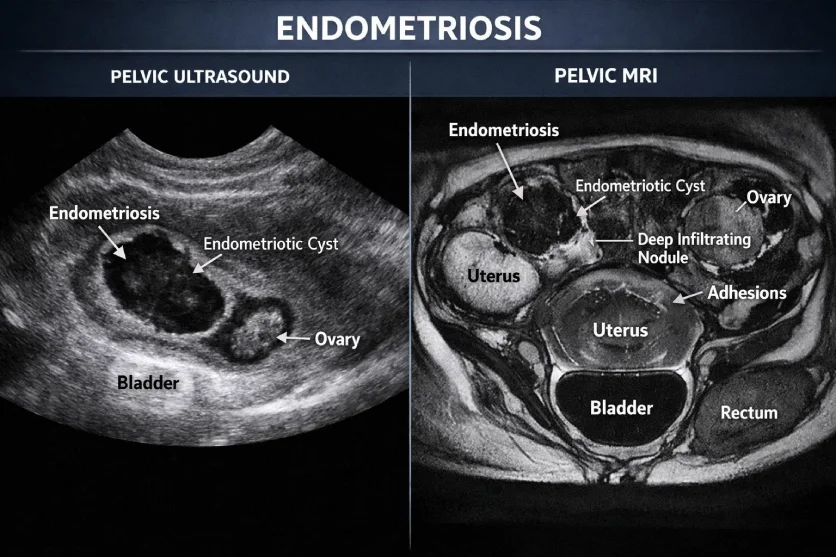
Can MRI detect endometriosis? Yes – when performed by experts, MRI is one of the most reliable imaging tools for detecting endometriosis, particularly in deep and complex cases. It uses magnetic fields to create detailed images of internal organs, allowing radiologists to identify even small or hidden lesions that are not visible through ultrasound or laparoscopy.
An Endometriosis MRI scan helps visualize ovarian endometriomas, adhesions, and deep infiltrating endometriosis (DIE) in regions like the bowel, bladder, or uterosacral ligaments. MRI’s ability to distinguish between different tissue types enables a clearer understanding of lesion depth and organ involvement, which is essential for planning surgery or non-surgical treatment.
Pelvic MRI for Endometriosis – What It Reveals
Pelvic MRI endometriosis scans are specialized studies focused on the pelvic region. These scans can detect:
- Ovarian cysts filled with old blood (endometriomas)
- Deep infiltrating nodules behind the uterus or in the rectovaginal space
- Pelvic adhesions that bind organs together
- Endometrial deposits affecting bowel or bladder walls
By providing a 3D anatomical view, pelvic MRI offers surgeons and gynecologists the information needed to assess disease severity and prepare individualized treatment strategies.
MRI Reading Parameters and Accuracy
For optimal visualization, radiologists use specific MRI sequences such as T1-weighted, T2-weighted, and fat-suppressed imaging. These sequences enhance the contrast between normal tissues and endometrial lesions, making even small abnormalities detectable.
Studies report MRI sensitivity for endometriosis detection between 90–95%, significantly higher than that of ultrasound in complex cases. This high diagnostic accuracy is why MRI is increasingly recognized as the best imaging for endometriosis – especially when performed by trained radiologists.
Why MRI Outperforms Other Imaging Methods
Unlike ultrasound, MRI is not limited by operator dependency or bowel gas interference. It provides comprehensive visualization of the entire pelvis, including areas that ultrasound cannot access. For patients with severe pain, prior surgeries, or suspected bowel involvement, MRI is the preferred non-invasive tool for diagnostic clarity.
At Mayflower Women’s Hospital, our radiology team utilizes advanced MRI protocols specifically designed for gynecologic imaging. Each MRI for endometriosis diagnosis is reviewed by a subspecialist radiologist, ensuring accuracy and early detection.
Endometriosis Ultrasound vs MRI: Which Is Better?
The Diagnostic Dilemma – Ultrasound or MRI?
Both ultrasound and MRI are valuable tools in identifying endometriosis, but they differ in accuracy, accessibility, and the level of detail they provide. Many women begin their diagnostic journey with endometriosis ultrasound because it’s cost-effective and widely available. However, while ultrasound can detect ovarian cysts (endometriomas) and larger abnormalities, it often misses subtle or deep lesions.
An Endometriosis MRI, on the other hand, provides a more comprehensive view of the pelvic region. It can identify tissue growths behind the uterus, near the bowel or bladder, and in the deeper layers of the pelvis – areas that are often difficult to evaluate with ultrasound. For complex cases, MRI delivers a complete anatomical map, making it invaluable for both diagnosis and surgical planning.
When Ultrasound Works Best
Ultrasound remains a reliable first-line investigation, especially for detecting:
- Ovarian endometriomas (chocolate cysts)
- Cysts larger than 2–3 cm
- Reproductive organ abnormalities
- Fluid accumulation or cystic structures
For superficial or easily visible lesions, endometriosis ultrasound provides sufficient information to guide treatment. It’s also ideal for routine follow-ups after treatment or surgery because of its speed and convenience.
When MRI Is the Right Choice
MRI is recommended when:
- Deep infiltrating endometriosis (DIE) is suspected
- The patient experiences severe pelvic pain despite normal ultrasound findings
- There’s suspected bowel, bladder, or ligament involvement
- Prior surgeries or adhesions complicate visualization
MRI for endometriosis diagnosis excels in identifying small lesions, scar tissue, and hidden adhesions that ultrasound can’t detect. In such cases, MRI offers the best imaging for endometriosis due to its high resolution and multi-planar capability.
Comparing Accuracy and Imaging Depth
| Parameter | Ultrasound | MRI |
|---|---|---|
| Accuracy for Ovarian Endometriomas | High | High |
| Detection of Deep Lesions (DIE) | Limited | Excellent |
| Bowel/Bladder Involvement | Poor | High |
| Operator Dependence | High | Low |
| Radiation Exposure | None | None |
| Cost | Lower | Moderate |
| Invasiveness | Non-invasive | Non-invasive |
While both tests are safe and radiation-free, MRI provides a more holistic and detailed assessment, making it the gold standard in complex or ambiguous cases.
Expert Insight – Combining Both for Best Results
In clinical practice, many specialists recommend starting with ultrasound and proceeding to MRI for confirmation. This layered approach ensures cost-effectiveness without compromising accuracy. At Mayflower Women’s Hospital, both imaging modalities are available within the same department, ensuring seamless diagnostic integration and faster reporting.
By aligning gynecologic expertise with radiologic precision, Mayflower provides patients with clear, evidence-based answers – helping them take control of their reproductive health sooner.
The Importance of Professional MRI Reading
Why Expertise Matters in MRI Interpretation
A high-quality MRI scan is only as effective as the expert who interprets it. While MRI machines generate detailed images of internal tissues, identifying endometriosis lesions requires advanced radiologic expertise and a deep understanding of pelvic anatomy. Subtle signs – such as small adhesions or faint signal differences – can easily be missed by general radiologists who are not trained in women’s imaging.
A professional MRI reading performed by an Endometriosis MRI specialist ensures accurate differentiation between normal anatomy, inflammation, scar tissue, and endometrial growths. This precision dramatically improves diagnostic reliability and guides the gynecologist toward the best course of treatment.
Common Errors in General MRI Interpretation
Non-specialized MRI readings may sometimes misclassify or overlook endometriotic lesions. Common challenges include:
- Confusing adhesions with bowel loops or fibrotic tissue
- Missing deep infiltrating endometriosis near the rectum or bladder
- Underestimating lesion size or extent due to limited field-of-view
- Failing to correlate radiologic findings with clinical symptoms
Such errors can delay proper diagnosis and extend a patient’s suffering. That’s why working with radiologists experienced in gynecologic MRI is critical for early and effective management.
Role of Endometriosis MRI Specialists
At Mayflower Women’s Hospital, our radiologists specialize exclusively in women’s imaging and endometriosis evaluation. Using tailored MRI protocols and advanced imaging sequences, they identify lesions as small as a few millimeters. Their focused approach ensures every MRI for endometriosis diagnosis delivers actionable insights that enable the gynecology team to craft personalized treatment plans.
The collaboration between the radiology and gynecology departments enhances care quality – bridging technology, expertise, and empathy for each patient’s unique experience.
How Expert Reading Improves Treatment Planning
When lesions are mapped precisely, surgeons can plan minimally invasive procedures more effectively, reducing surgical time and improving fertility outcomes. In non-surgical cases, accurate MRI findings help physicians recommend hormonal therapies or pain management strategies that directly target affected regions.
At Mayflower, this integrated model of professional interpretation and multidisciplinary collaboration ensures that each patient receives the most efficient, evidence-based treatment path possible.
Step-by-Step: What Happens During an Endometriosis MRI Scan
Preparing for the Scan
Before undergoing an Endometriosis MRI scan, patients receive clear pre-scan instructions to ensure the highest-quality results. Typically, the scan is scheduled between the 8th and 12th day of the menstrual cycle, when pelvic structures are most visible and endometrial activity is easier to assess.
Patients are advised to:
- Avoid eating heavy meals two hours before the scan.
- Empty the bladder partially to maintain comfort and visibility.
- Inform the technician about any metal implants, pacemakers, or prior surgeries.
At Mayflower Women’s Hospital, patient comfort is a top priority. The environment is calm, and the entire process is handled by a specialized radiology team trained in women’s imaging.
What to Expect During a Pelvic MRI for Endometriosis
During the procedure, the patient lies on the MRI table, which slides into a circular scanner. Unlike CT scans or X-rays, MRI uses magnetic waves – meaning there is no radiation exposure. The scan typically lasts 30–45 minutes.
A contrast agent may be administered in certain cases to enhance visualization of lesions, adhesions, or endometrial implants. The machine makes rhythmic tapping sounds, but noise-canceling headphones or earplugs are provided to ensure relaxation.
The pelvic MRI for endometriosis captures multiple imaging sequences (T1, T2, and fat-suppressed views) that provide detailed anatomical information. These images help identify even small endometriotic nodules that might otherwise remain invisible through ultrasound.
After the Scan – Reading and Reporting Process
Once the MRI is completed, the images are analyzed by a radiologist specializing in endometriosis. The expert examines tissue characteristics, lesion size, and exact locations in relation to organs such as the uterus, bowel, or bladder.
At Mayflower, this process involves a dual-review system – each scan is verified by a senior Endometriosis MRI specialist to ensure accuracy. The report is then shared with the gynecology team, who integrate findings into a comprehensive treatment plan.
This professional collaboration ensures that every patient benefits from non-invasive endometriosis diagnosis without unnecessary exploratory surgery.
Patient Comfort and Care at Mayflower
Mayflower Hospital places equal emphasis on diagnostic precision and patient well-being. Our imaging suites are designed with privacy and comfort in mind, allowing patients to remain calm throughout the scan. Radiologists and technologists guide each step, explaining procedures clearly to reduce anxiety and build trust.
This compassionate, expert-led approach not only enhances diagnostic outcomes but also makes the experience empowering for women seeking answers about their health.
MRI vs Laparoscopy: Shifting to Non-Invasive Endometriosis Diagnosis
Laparoscopy – The Traditional Gold Standard
For decades, laparoscopy has been considered the gold standard for diagnosing endometriosis. This minimally invasive surgical procedure involves inserting a small camera through an abdominal incision to directly view the pelvic organs. It allows surgeons to visualize and even remove endometrial lesions in a single session.
However, laparoscopy, despite its effectiveness, comes with certain challenges:
- It requires anesthesia and a recovery period.
- There is a small risk of complications such as infection or bleeding.
- It may not always detect microscopic or hidden lesions in complex cases.
These limitations have encouraged specialists to explore safer, more accessible diagnostic tools that reduce patient discomfort and risk.
MRI – A Game-Changer in Non-Invasive Diagnosis
With advances in medical imaging, MRI for endometriosis diagnosis now provides a non-surgical alternative that offers near-surgical accuracy. It allows physicians to assess the extent, depth, and location of lesions without making any incisions.
A well-performed Endometriosis MRI scan can:
- Identify deep infiltrating endometriosis (DIE)
- Detect lesions near the bowel, bladder, and ligaments
- Map adhesions and organ displacement
- Help surgeons plan targeted laparoscopic or robotic interventions only when necessary
MRI not only reduces the need for diagnostic surgery but also ensures that, if surgery is needed, it’s more precise and less invasive.
Benefits of MRI Over Laparoscopy
| Parameter | MRI | Laparoscopy |
|---|---|---|
| Invasiveness | Non-invasive | Minimally invasive (requires surgery) |
| Anesthesia Needed | No | Yes |
| Recovery Time | None | 1–2 weeks |
| Risk of Complications | None | Possible (infection, bleeding) |
| Diagnostic Accuracy | High (especially with expert reading) | Very high |
| Therapeutic Capability | Diagnostic only | Diagnostic + surgical treatment |
| Cost-Effectiveness | Moderate | Higher (hospital & anesthesia costs) |
When combined with clinical evaluation and ultrasound, MRI can often eliminate the need for unnecessary exploratory procedures. It allows doctors to focus directly on treatment – saving time, cost, and discomfort for the patient.
The Future of Non-Invasive Endometriosis Diagnosis
The global medical community is increasingly shifting toward non-invasive endometriosis diagnosis techniques. MRI, when performed by specialists and correlated with clinical symptoms, provides comprehensive insights that once required surgical confirmation.
At Mayflower Women’s Hospital, this modern diagnostic pathway has already transformed care outcomes for women dealing with chronic pelvic pain or infertility. With a focus on precision, comfort, and patient education, our imaging team ensures every diagnosis is accurate and empowering.
Why Choose Mayflower Hospital for Endometriosis MRI

Expertise That Ensures Diagnostic Accuracy
At Mayflower Women’s Hospital, every Endometriosis MRI is conducted and reviewed by highly trained radiologists specializing in women’s imaging. Our team understands that detecting endometriosis requires precision, experience, and a deep understanding of pelvic anatomy. By using advanced imaging protocols tailored for gynecologic evaluation, Mayflower ensures that even subtle lesions and adhesions are detected with clarity and accuracy.
Unlike general diagnostic centers, Mayflower’s approach integrates radiology with gynecology – creating a unified diagnostic process. The Endometriosis MRI specialists collaborate closely with gynecologists to interpret results in the clinical context of each patient, ensuring personalized and effective treatment plans.
Advanced Technology and Specialized MRI Protocols
Mayflower Hospital is equipped with state-of-the-art MRI scanners designed for high-resolution pelvic imaging. The technology allows radiologists to:
- Perform pelvic MRI endometriosis scans with enhanced contrast and anatomical detail.
- Identify deep infiltrating endometriosis and hidden lesions.
- Generate 3D images for surgical planning and mapping of adhesions.
Every MRI for endometriosis diagnosis follows a customized protocol based on the patient’s history, pain pattern, and suspected disease severity. This ensures the most informative and reliable outcome possible – minimizing false negatives and eliminating diagnostic uncertainty.
Integrated, Multidisciplinary Care
Mayflower’s diagnostic and gynecologic departments work hand in hand to provide complete patient-centered care. Radiologists and gynecologists jointly review MRI findings, enabling faster correlation between imaging results and symptoms.
This collaboration helps in:
- Accurate treatment planning (medical or surgical)
- Targeted fertility management
- Minimizing unnecessary exploratory procedures
Patients benefit from comprehensive counseling after diagnosis, ensuring they understand their condition and next steps in treatment.
Trusted by Patients Across India
Mayflower Hospital has established itself as a trusted destination for non-invasive endometriosis diagnosis in India. Our combination of compassionate care, cutting-edge technology, and expert reporting has helped thousands of women achieve clarity and relief after years of uncertainty.
Each scan is reviewed with empathy and precision – two values that define Mayflower’s approach to women’s health. Whether it’s a first-time evaluation or a second opinion, patients can expect transparency, accuracy, and comfort every step of the way.
Book Your Endometriosis MRI Scan
If you are experiencing unexplained pelvic pain, irregular cycles, or infertility, an Endometriosis MRI scan at Mayflower could be the first step toward accurate diagnosis and better health outcomes.
Schedule your MRI scan today to receive an expert evaluation from our diagnostic team. Experience world-class imaging, personalized attention, and evidence-based guidance at Mayflower Women’s Hospital, Ahmedabad-a leader in women’s healthcare and diagnostic excellence.
Preparing for Your Endometriosis MRI Appointment
Why Preparation Matters
Proper preparation before an Endometriosis MRI scan ensures optimal image clarity and diagnostic accuracy. Since the pelvic organs can shift or vary depending on the menstrual cycle and bowel activity, following certain pre-scan guidelines helps radiologists obtain the clearest possible images. At Mayflower Women’s Hospital, patients receive personalized instructions before every MRI appointment to ensure maximum comfort and accuracy.
Pre-Scan Instructions
Here are some key steps patients are advised to follow before their MRI for endometriosis diagnosis:
- Timing: The scan is ideally scheduled between the 8th and 12th day of the menstrual cycle for best visibility.
- Diet: Avoid eating heavy meals 2–3 hours before the scan. Light meals or liquids are acceptable.
- Bowel Preparation: Some patients may be asked to empty their bowels to reduce interference in pelvic imaging.
- Clothing & Accessories: Wear loose, comfortable clothing and avoid metallic items like jewelry, zippers, or watches.
- Medical History: Inform your radiologist if you have any implants, pacemakers, or prior pelvic surgeries.
Patients who are anxious about the procedure can request a short orientation with the imaging team for reassurance and to clarify any concerns.
During the Scan
Once inside the MRI suite, you will lie comfortably on the scanner table. The technologist positions you carefully to capture all necessary pelvic angles. You’ll hear rhythmic tapping or humming noises during the scan – these are normal sounds produced by the MRI machine.
For pelvic MRI endometriosis, contrast dye may sometimes be used to enhance visualization of lesions or adhesions. The process is completely safe and typically takes 30–45 minutes. Throughout the scan, a technician monitors you closely and maintains communication to ensure comfort.
After the Scan – What Happens Next
After the scan, you can resume normal activities immediately. The images are sent to an Endometriosis MRI specialist for detailed interpretation. A comprehensive report is then shared with your gynecologist, usually within 24–48 hours.
At Mayflower Women’s Hospital, this report review includes a multidisciplinary discussion between radiologists and gynecologists to ensure the findings align with your symptoms and medical history. This coordinated approach enhances treatment accuracy and patient outcomes.
Comfort and Care at Every Step
Mayflower Hospital prioritizes both medical precision and emotional comfort. Our imaging staff ensures a calm, patient-friendly atmosphere during every Endometriosis MRI scan. Women who may feel anxious are offered clear communication, supportive staff presence, and guided breathing techniques for relaxation.
Every step – from preparation to reporting – is designed to deliver a seamless, stress-free experience while ensuring the highest diagnostic standards in non-invasive endometriosis diagnosis.
Conclusion – Empowering Women with Accurate, Non-Invasive Diagnosis
Endometriosis is a complex and often misunderstood condition that requires more than just medical treatment – it demands precise, compassionate, and expert-driven diagnosis. The evolution of Endometriosis MRI has transformed how doctors detect and manage this condition, offering women a faster, safer, and non-invasive endometriosis diagnosis alternative.
Unlike traditional exploratory surgery, MRI provides a clear window into the pelvic region, revealing lesions, adhesions, and organ involvement with remarkable detail. When interpreted by an experienced Endometriosis MRI specialist, these insights allow doctors to plan targeted treatments that restore comfort, fertility, and overall well-being.
At Mayflower Women’s Hospital, our commitment to diagnostic excellence extends beyond technology. We combine advanced MRI for endometriosis diagnosis with personalized care, ensuring every woman receives clarity, accuracy, and confidence in her health journey. From early symptom evaluation to advanced imaging and treatment coordination, our specialists are with you every step of the way.
If you suspect you may have endometriosis – or have struggled with unclear test results – consider scheduling your Endometriosis MRI scan at Mayflower. Discover the difference that professional expertise and precision imaging can make in reclaiming your health and quality of life.
FAQs
Yes. MRI for endometriosis diagnosis is more detailed and precise than ultrasound, especially for detecting deep infiltrating endometriosis (DIE) that affects the bowel, bladder, or ligaments. Ultrasound is useful for identifying ovarian cysts but may miss smaller or hidden lesions that MRI can detect clearly.
The best imaging for endometriosis depends on the complexity of the case. In general, MRI provides superior clarity and depth, making it the preferred method for non-invasive diagnosis. When interpreted by an Endometriosis MRI specialist, it offers up to 95% accuracy in identifying lesions and adhesions.
No. The Endometriosis MRI scan is entirely non-invasive and painless. You may feel mild discomfort from lying still during the scan or from the contrast injection (if used), but there is no physical pain involved. Mayflower’s imaging rooms are designed to ensure a comfortable, calm experience.
In some cases, contrast dye is used to highlight inflammation, cysts, or lesions more clearly. It helps radiologists differentiate between endometriotic tissue and other pelvic structures. Your doctor will decide whether contrast is necessary based on your medical history and prior imaging results.
MRI is highly effective in identifying moderate to severe endometriosis. While very mild or microscopic lesions might still go undetected, advanced imaging protocols at Mayflower Women’s Hospital enhance detection rates significantly. When MRI is combined with clinical evaluation and ultrasound, diagnostic accuracy increases even further.
An ultrasound can detect endometriosis to some extent – especially ovarian cysts (endometriomas) and superficial lesions. However, its limitations in visualizing deep or hidden areas make it less comprehensive than MRI. For this reason, doctors often recommend both imaging modalities for a full assessment.
Avoid heavy meals two hours before your scan, wear comfortable clothing without metal, and schedule the test between the 8th and 12th day of your menstrual cycle. MRI in the Diagnosis of Endometriosis. These small steps ensure a clearer image and a smoother diagnostic experience.
Mayflower Women’s Hospital is a trusted leader in non-invasive endometriosis diagnosis, equipped with the latest MRI technology and led by expert radiologists. The hospital’s integrated gynecology and radiology teams ensure accurate readings, faster diagnosis, and personalized treatment plans.
Author
-

Dr. Smeet, true to his name, is known for his warm personality and cheerful smile that make patients instantly feel at ease with him.
Until now, he has performed 8000+ surgeries and several of which are supra-major surgeries for deep infiltrating endometriosis and fertility enhancing surgeries. With several publications in notable journals, he is constantly pushing the envelope of possibilities in gynecological surgeries