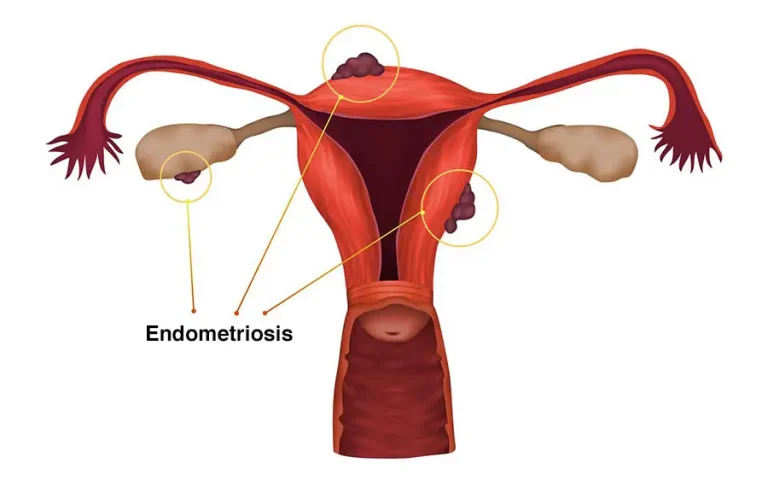
Endometriosis symptoms often begin as severe period pain and can evolve into daily discomfort that affects work, relationships, and fertility. Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, causing inflammation, scarring, and sometimes infertility—see the succinct WHO definition for context.
What is endometriosis?
Endometriosis can start around the first period and persist until menopause, affecting roughly 1 in 10 people of reproductive age. For a quick primer, compare our plain-English overview with the Mayo Clinic’s symptoms page; both highlight pain and infertility as common presentations.
At Mayflower, readers can move from learning to action via our in-depth Endometriosis information page and the dedicated Endometriosis Clinic in Ahmedabad for specialist evaluation.
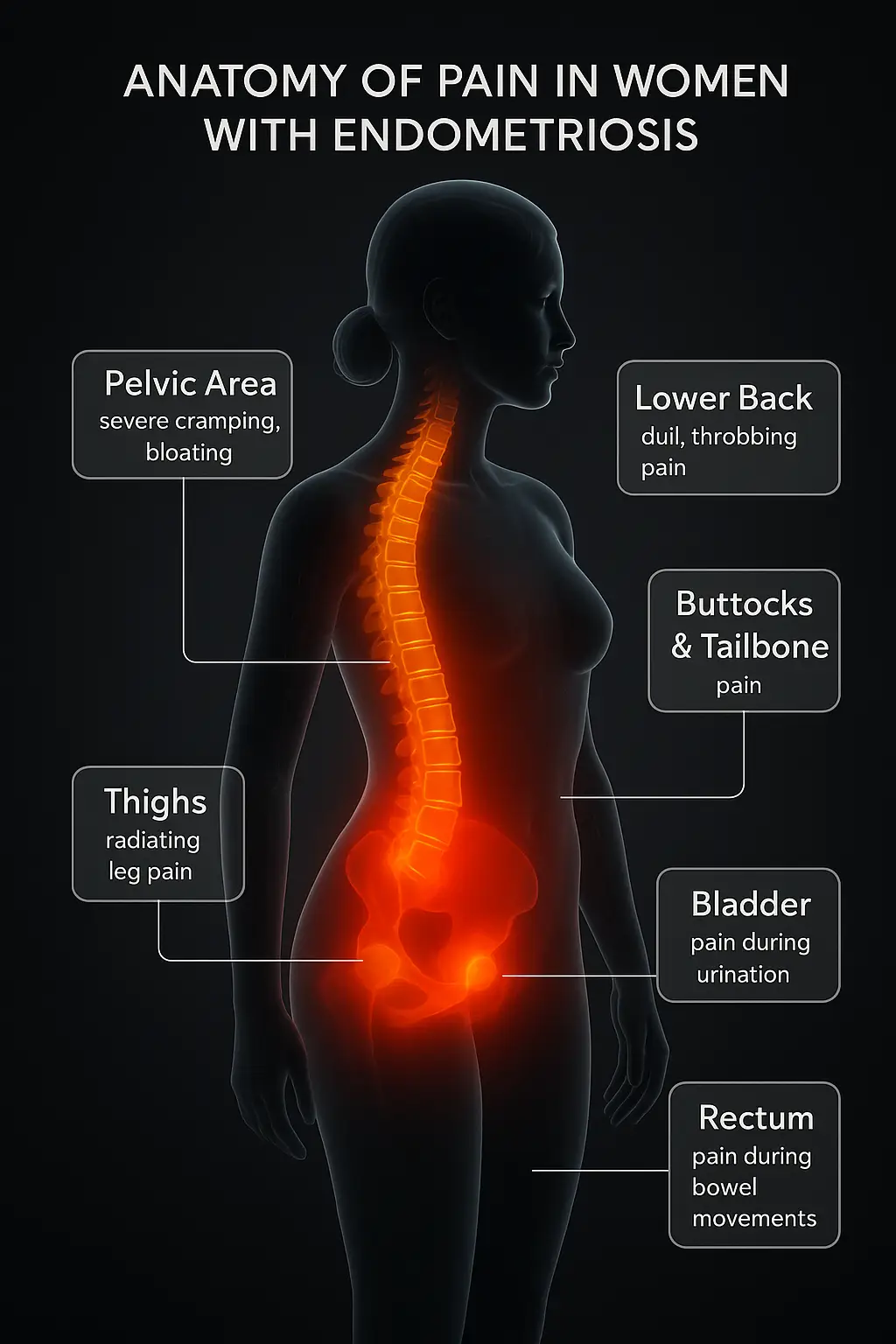
Symptom checklist & the “pain map”
Think in patterns, not single symptoms. Typical endometriosis pain areas include the lower abdomen/pelvis and lower back; pain may radiate to the hips or legs. Many describe pain that starts before bleeding and lingers after. Pain during sex (deep dyspareunia), bowel or urinary symptoms around periods, heavy or irregular bleeding, bloating, nausea, fatigue, and reduced quality of life are common—this mirrors the Mayo Clinic’s symptom list.
If you see yourself here, book a review with our Gynaecology Department for structured evaluation and triage.
Endometriosis symptoms in teens
Teens can have the same disease pattern but present as “periods that keep them home,” severe cramps unresponsive to OTC meds, or cycling GI/urinary symptoms. The American College of Obstetricians and Gynecologists advises considering endometriosis when pain persists despite first-line care—see ACOG’s adolescent guidance for red flags.
For teens missing school due to pain, consider an early consult at our Endometriosis Clinic to reduce delays.
Endometriosis causes & risk factors
There’s no single cause. Evidence points to a multifactorial model—hormonal (estrogen-driven), immune and inflammatory pathways, genetics, and retrograde menstruation. The recent WHO Bulletin review summarizes mechanisms and highlights how uncertainty contributes to diagnosis delays globally. Family history, early menarche, short cycles, and heavy bleeding may raise risk, but none alone confirm disease.
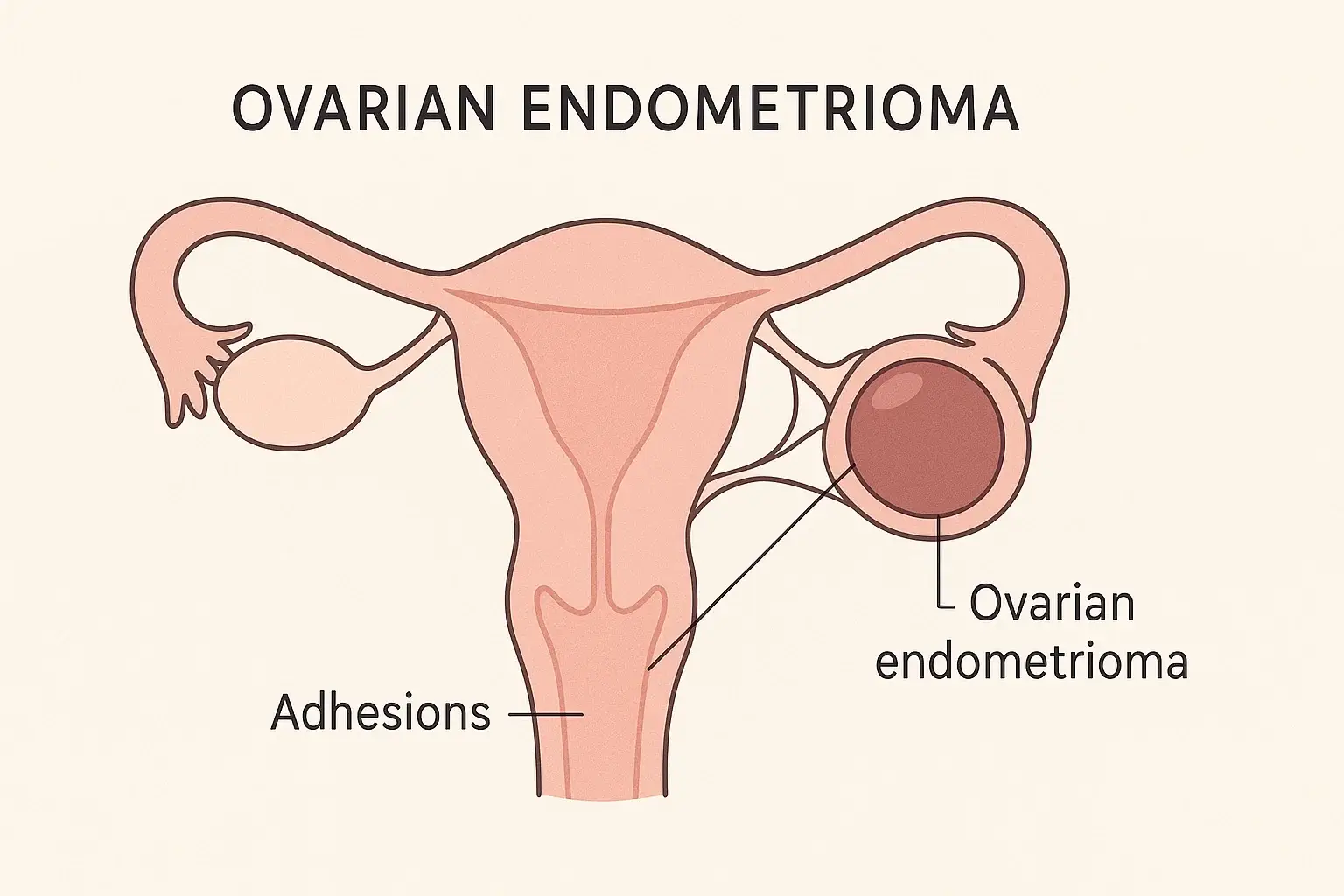
“Chocolate cyst” (ovarian endometrioma) explained
An ovarian endometrioma—often called a chocolate cyst—is a blood-filled cyst on the ovary caused by endometriosis. Patients may notice persistent pelvic pain, painful periods, painful sex, and fertility challenges. Sonography often shows characteristic features; MRI helps in complex cases and pre-surgical planning. For clinical framing, compare our approach with the Cleveland Clinic’s explainer and Mayo’s diagnosis/treatment page.
When an endometrioma is suspected, our Extensive Diagnosis pathway integrates focused ultrasound and MRI with fertility goals before discussing surgery.
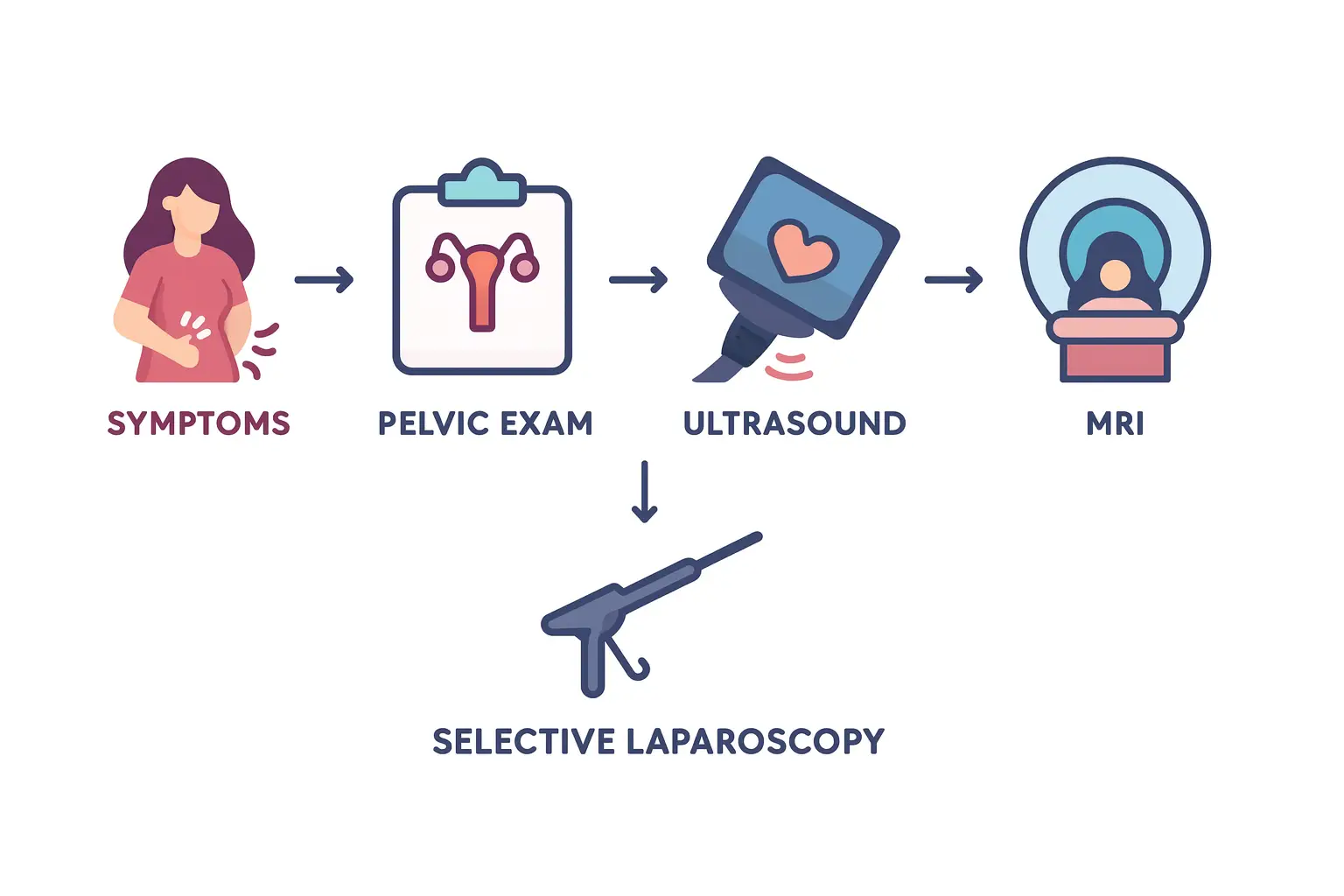
How is endometriosis diagnosed?
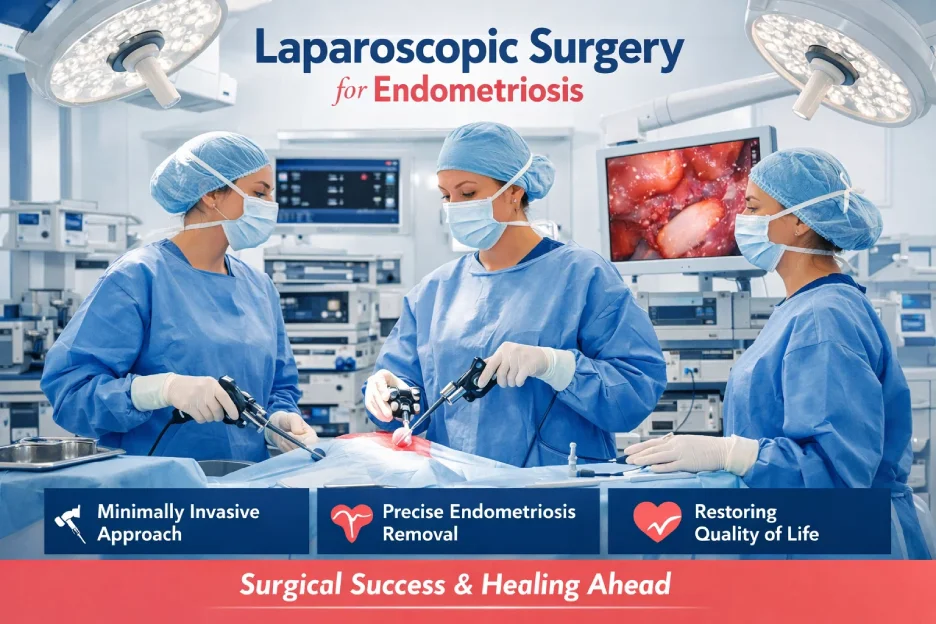
How is endometriosis diagnosed? We start with symptoms and history, then a pelvic exam and targeted imaging. To reduce endometriosis diagnosis delay, modern pathways emphasize imaging and empirical treatment when appropriate. The 2022 ESHRE guideline states that diagnosis can be made without laparoscopy in many cases; laparoscopy is recommended when imaging is negative or treatment fails/doesn’t fit.
At Mayflower, first-line transvaginal ultrasound screens for endometriomas and many deep lesions; MRI maps deep infiltrating endometriosis (DIE), bowel/bladder involvement, and surgical planes. For difficult cases or second opinions, patients use our MRI Scan Reading and Read My Endo MRI services to guide next steps. Compare this to the NHS overview for testing expectations.
Ultrasound vs MRI vs Laparoscopy—what each adds
- Ultrasound is widely available and detects endometriomas and many DIE nodules when performed by experienced operators.
- MRI refines mapping for complex disease, especially rectovaginal or bowel involvement, and informs surgical planning.
- Laparoscopy allows visualization and treatment with biopsy confirmation; per ESHRE 2022, it’s not the routine “gold standard” for every patient but is reserved for selected scenarios. ACOG materials for patients still explain laparoscopy as the way to be certain—useful for counseling balance.
Endometriosis stages (I–IV): what staging means—and doesn’t
The ASRM stages describe how much disease is seen, where it’s found, and whether adhesions are present. Staging isn’t a pain score—people with “mild” disease can have severe pain and vice versa. Treatment depends more on symptoms, goals (e.g., pregnancy), and site (e.g., rectovaginal DIE) than on stage alone; the Cleveland Clinic overview makes this distinction clear.
Endometriosis vs adenomyosis (quick comparison)
Both involve uterine-like tissue, but the location differs. Endometriosis grows outside the uterus (e.g., ovaries, peritoneum, bowel), while adenomyosis grows within the uterine muscle. Both can cause heavy, painful periods; adenomyosis more often enlarges the uterus and causes diffuse cramping. Ultrasound is the first step for both; MRI clarifies complex cases—see the NHS guide for patient-friendly distinctions.
Endometriosis and infertility—what to expect
Endometriosis can affect fertility via inflammation, adhesions, and endometriomas altering ovarian reserve or tubal movement. Options range from pain control and hormonal suppression to laparoscopic excision in selected cases, and fertility treatments when appropriate—see Mayo’s treatment overview alongside our IVF program to understand the care continuum. If you’re actively trying to conceive, coordinate between the Endometriosis Clinic and our IVF Centre for a unified plan.
When to see a doctor (red flags)
Book a visit if pain interrupts work or school, if periods are worsening, if sex or bowel/urinary function are painful, or if you’ve been trying to conceive for 12 months (6 months if over 35). If bowel, bladder, or ureter symptoms cycle with your period, ask about imaging for DIE. For a quick appointment, use our Book an Appointment page or start with the Gynaecology Department. The NHS page lists similar thresholds, which we follow in clinic.
Awareness & next steps
March is endometriosis awareness month—a good nudge to track symptoms, log pain days, and plan reviews. If you recognize the patterns above, move from searching to scheduling; our Patients Centre has practical info for travel and planning. For broader context and lived experiences, see global coverage (e.g., WHO fact sheet) and ongoing public stories that keep awareness high.
FAQ
Severe period pain, pain that starts before bleeding and lingers after, pain with sex, bowel/urinary discomfort around periods, heavy or irregular bleeding, fatigue; sometimes difficulty conceiving. See Mayo’s list.
Yes. Transvaginal ultrasound detects endometriomas and many deep lesions in experienced hands; MRI refines mapping. ESHRE 2022 explains where each fits in diagnosis.
Not for everyone. Per ESHRE 2022, laparoscopy is reserved when imaging is negative or treatment fails/doesn’t suit.
No. Many conceive naturally. When it does affect fertility, a plan aligning symptom control, surgery (in selected cases), and fertility treatment can help; see Cleveland Clinic’s overview.
Pain control, hormonal therapy, and surgery for selected cases; fertility treatments when pregnancy is the goal. Compare your options against Mayo’s treatment page.