Hormonal therapy for endometriosis plays a crucial role in managing pain, reducing inflammation, and controlling the abnormal growth of endometrial tissue. For many women, it is one of the most effective non-surgical options to improve quality of life and delay disease progression.
Endometriosis is a condition where tissue similar to the uterine lining grows outside the uterus, often causing chronic pelvic pain, heavy periods, and fertility challenges. Because these tissues respond to hormonal changes, regulating hormones becomes a vital part of treatment.
At Mayflower Women’s Hospital, our gynecology specialists use an evidence-based, personalized approach to hormonal management – balancing efficacy with safety. Whether it’s birth control pills, progesterone therapy, or GnRH agonists, the right hormonal therapy can help control symptoms and support long-term well-being.
In this blog, we’ll explain how hormonal therapy works, its different options, potential side effects, and what you can expect from treatment at Mayflower.
Understanding Endometriosis and Hormonal Imbalance
Hormones play a powerful role in regulating the menstrual cycle – and when they become imbalanced, endometriosis symptoms can worsen. In women with endometriosis, estrogen often acts as the primary driver for tissue growth outside the uterus. The result is inflammation, pelvic pain, and sometimes, fertility challenges.
Endometriosis hormone treatment works by restoring balance between estrogen and progesterone. Estrogen encourages the endometrial tissue to thicken, while progesterone helps limit that growth. When progesterone levels are low or estrogen levels remain unchecked, the tissue continues to build up and bleed with every cycle, leading to painful symptoms.
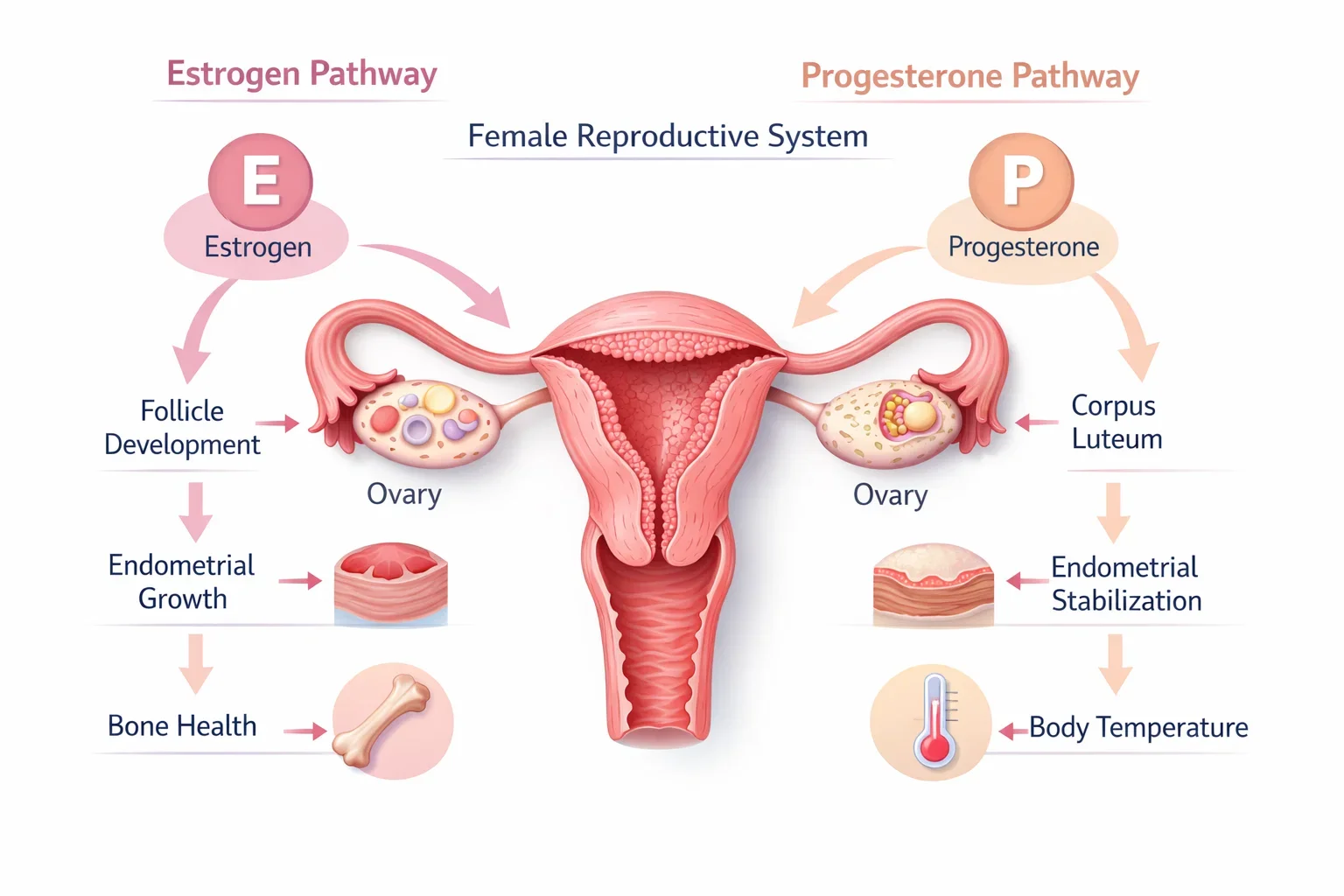
Over time, this imbalance can also cause hormones for endometriosis pain to fluctuate irregularly – which is why patients may experience cyclical discomfort, bloating, or fatigue. These hormonal shifts are also responsible for many endometriosis side effects, such as mood swings or heavy bleeding.
Understanding this connection is key: by controlling estrogen and supporting progesterone, hormonal therapy targets the disease at its root cause. This sets the stage for more advanced treatment options discussed in the next section.
What Is Hormonal Therapy for Endometriosis?
Hormonal therapy for endometriosis is a medical approach that uses hormones to reduce pain, control bleeding, and slow the growth of endometrial tissue outside the uterus. Since endometriosis is fueled by estrogen, these therapies work by suppressing or balancing hormone levels in the body to minimize inflammation and prevent tissue buildup.
Unlike surgical options that remove existing lesions, hormonal therapy focuses on managing symptoms and preventing new growth. It helps make menstrual cycles lighter, shorter, or sometimes even pauses them temporarily, giving the body a chance to heal and reducing chronic discomfort.
Endometriosis treatment options under hormonal therapy vary depending on the severity of symptoms, age, and fertility goals. Some patients respond best to oral contraceptives, while others benefit from advanced hormone-regulating medications like GnRH agonists or progesterone-based therapies.
At Mayflower Women’s Hospital, specialists tailor each hormonal plan to the patient’s unique hormonal profile. Through regular monitoring, dosage adjustments, and supportive care, they ensure treatment remains safe, effective, and aligned with the patient’s long-term health goals.
Types of Hormonal Treatments for Endometriosis

No single treatment fits every woman with endometriosis. The right hormonal therapy depends on your symptoms, goals, and how your body responds to specific hormones. Below are the most common and medically approved endometriosis hormone treatment options that gynecologists recommend.
Combined Oral Contraceptives (Birth Control Pills)
One of the first-line treatments for endometriosis is birth control for endometriosis, commonly known as combined oral contraceptives. These pills contain synthetic versions of estrogen and progesterone that work together to suppress ovulation and stabilize hormonal fluctuations.
By preventing the monthly surge of estrogen, birth control pills help reduce menstrual pain, lighten bleeding, and limit the growth of endometrial tissue. Many women also find that continuous pill use helps avoid painful periods entirely.
However, it’s important to take these medications under medical supervision, as not all formulations suit every patient.
Progestin and Progesterone Therapy
Progesterone therapy for endometriosis helps counteract estrogen’s stimulating effect on endometrial tissue. By increasing progesterone levels, this therapy prevents ovulation and thins the uterine lining, reducing inflammation and pain.
Common forms include oral tablets, injections, or intrauterine devices (IUDs) that release a steady amount of progestin. Some women prefer IUDs for long-term control, as they are effective for up to five years.
While progesterone therapy is generally well tolerated, mild side effects such as bloating, mood changes, or irregular bleeding can occur – all manageable with timely doctor review.
GnRH Agonists and Antagonists
GnRH agonist endometriosis therapy is a more advanced option often prescribed when other hormonal treatments aren’t sufficient. These medications temporarily suppress the ovaries’ production of estrogen, creating a reversible “menopause-like” state.
The reduction in estrogen helps shrink endometrial implants and relieve pain significantly. However, since low estrogen can cause hot flashes and bone density loss, doctors often recommend “add-back” therapy – small doses of estrogen or progesterone to balance side effects.
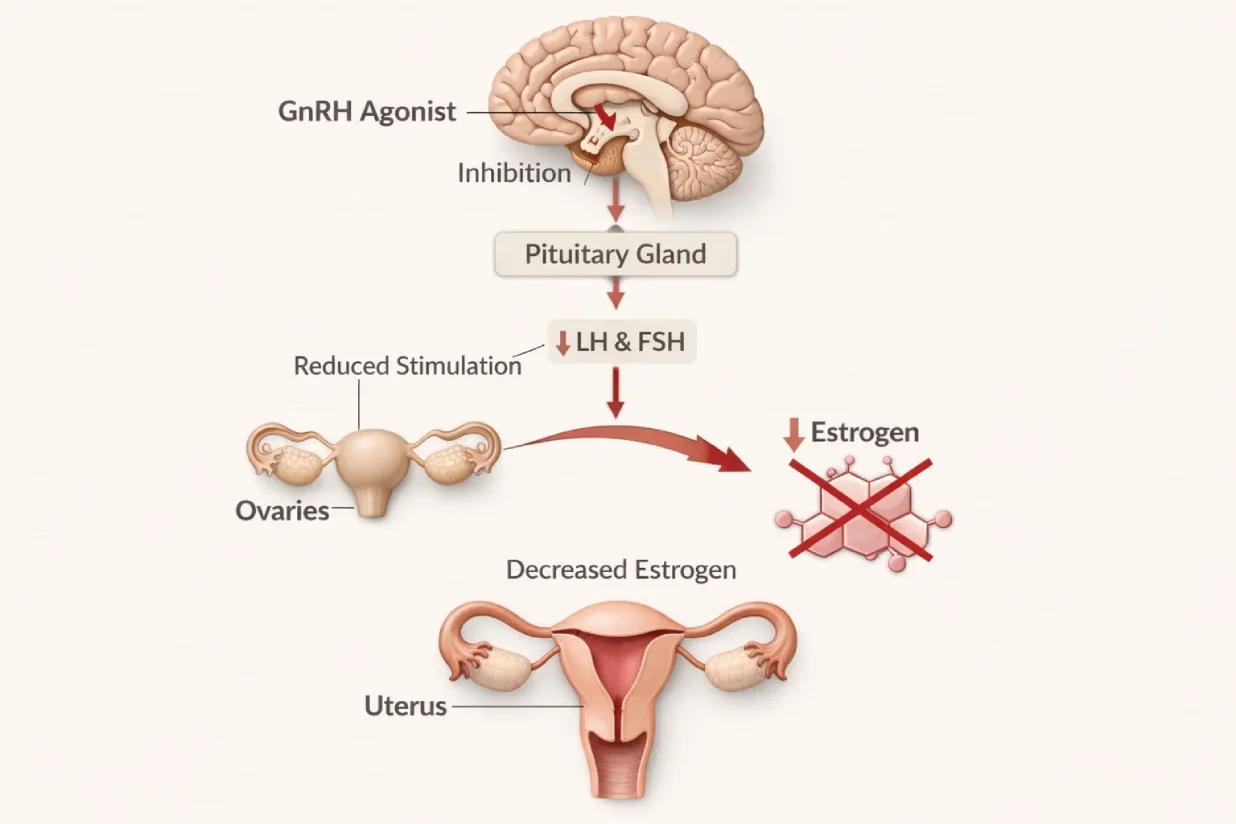
Newer GnRH antagonists, such as elagolix, offer shorter treatment durations with fewer side effects, making them a preferred option in some cases.
Other Hormonal Agents (Danazol, Aromatase Inhibitors, etc.)
For women who don’t respond well to standard therapies, doctors may consider other hormonal agents like danazol or aromatase inhibitors.
Danazol suppresses estrogen production but may cause androgenic side effects such as acne or weight gain. Aromatase inhibitors work by blocking estrogen synthesis in the body, helping manage severe or resistant endometriosis cases.
Because of their potency, these medications are typically used under strict medical supervision and only for limited periods.
Each hormonal option comes with unique benefits and considerations. While they help control pain and inflammation, side effects are common and vary by treatment type. Understanding and managing these effects is the key to achieving the best outcomes – which we’ll explore next.
Managing Side Effects of Endometriosis Hormonal Therapy
While hormonal therapy for endometriosis is highly effective in controlling pain and slowing disease progression, some patients may experience mild to moderate side effects. These reactions vary depending on the type of hormone used, dosage, and individual tolerance. Understanding these effects-and managing them proactively-ensures safer, long-term treatment outcomes.
Common Side Effects
Most women tolerate hormonal therapy well, but it’s normal to experience temporary changes such as:
- Irregular spotting or missed periods
- Mood swings or irritability
- Weight fluctuations
- Headaches or fatigue
- Hot flashes, especially during GnRH agonist endometriosis treatment
These side effects often subside as the body adjusts to new hormone levels. In some cases, your doctor may modify the dosage or change the medication type to improve comfort.
How to Manage Hormonal Therapy Side Effects
- Stay consistent with medication: Irregular intake can worsen side effects.
- Adopt an anti-inflammatory diet: Including omega-3 fats, leafy greens, and whole grains supports hormonal balance.
- Regular exercise: Light workouts and yoga can reduce stress-related hormonal fluctuations.
- Follow-up visits: Regular monitoring helps doctors adjust your treatment for minimal discomfort.

At Mayflower Women’s Hospital, patients receive continuous monitoring to minimize endometriosis hormonal therapy side effects. Our team ensures that therapy remains personalized, safe, and effective throughout every phase of recovery.
Though side effects can occur, they are manageable with medical guidance and lifestyle support. The next step is understanding how hormonal therapy compares to other endometriosis treatment options-and when it might be the right choice for you.
Hormonal Therapy vs Other Endometriosis Treatment Options
Endometriosis treatment requires a personalized, multi-layered approach – there’s no one-size-fits-all solution. Hormonal therapy for endometriosis is often compared with other medical and surgical options to determine the best fit for each patient’s symptoms and fertility goals.
Hormonal Therapy vs Surgical Treatment
Hormonal therapy helps manage symptoms and prevent recurrence, while surgery removes visible endometrial lesions.
- Best for: Patients with mild to moderate pain or those planning pregnancy later.
- Procedure: Non-invasive, relies on oral or injectable medications.
- Recovery: Minimal downtime, gradual symptom improvement.
In contrast, laparoscopic surgery may be recommended when hormonal therapy doesn’t provide sufficient relief or when cysts and adhesions interfere with fertility. Mayflower’s surgeons specialize in minimally invasive endometriosis excision, ensuring faster recovery and minimal scarring.
Hormonal Therapy vs Natural and Supportive Options
Some women explore complementary therapies like diet modifications, supplements, or physiotherapy. While these approaches can reduce inflammation and improve comfort, they work best when combined with medical treatment.
Lifestyle adjustments-especially following an anti-inflammatory diet and regular physical activity-can enhance the results of hormone-based care.
Choosing the Right Combination
The ideal treatment often involves a combination of hormonal therapy and surgical management, guided by a gynecologist. At Mayflower Women’s Hospital, patients receive customized treatment pathways that combine hormonal regulation, nutritional support, and pain management for sustainable relief.
Once you understand the benefits and limitations of each option, the next question becomes: how do you know if hormonal therapy is right for you? Let’s explore how specialists decide which patients benefit most.
Is Hormonal Therapy Right for You?
Not every woman with endometriosis requires hormonal therapy, but for many, it’s a key part of achieving long-term relief and improved quality of life. Understanding whether you’re an ideal candidate depends on your medical history, symptom pattern, and personal goals – especially around fertility.
When Hormonal Therapy Is Recommended
Doctors often suggest hormonal treatment when:
- You have chronic pelvic pain or heavy menstrual bleeding.
- Imaging or laparoscopy confirms early or moderate endometriosis.
- You’re not planning pregnancy immediately.
- Previous pain medications or natural remedies haven’t provided adequate relief.
In such cases, regulating estrogen levels can significantly reduce inflammation, tissue growth, and monthly discomfort.
When It May Not Be Suitable
Hormonal therapy might not be the first choice if:
- You have a history of blood clots, migraines, or liver conditions.
- You’re actively trying to conceive.
- You’ve previously experienced severe side effects from hormonal medications.
In these scenarios, your doctor may explore alternative treatments such as laparoscopic surgery, lifestyle therapy, or natural interventions.
Diagnostic Evaluation Before Starting Therapy
Before prescribing any medication, Mayflower’s specialists conduct a detailed evaluation that may include:
- Pelvic MRI or ultrasound to assess endometrial spread.
- Hormonal blood tests to identify imbalance levels.
- Laparoscopy results (if available) to gauge disease severity.
These diagnostic steps ensure that the prescribed plan aligns precisely with your body’s hormonal profile – maximizing effectiveness and minimizing side effects.
Once the treatment plan is defined, most patients naturally wonder about timelines and costs. Let’s look at how long hormonal therapy typically lasts and what influences its cost in India.
Hormonal Treatment Endometriosis Cost and Duration
When planning hormonal therapy for endometriosis, understanding both cost and treatment duration helps set realistic expectations. At Mayflower Women’s Hospital, every treatment plan is designed to balance clinical effectiveness with affordability and long-term safety.
Average Cost of Hormonal Therapy
The hormonal treatment endometriosis cost in India varies depending on the type of medication and duration of use.
- Oral contraceptive pills: ₹500–₹1,500 per month
- Progesterone injections or IUDs: ₹2,000–₹10,000 (depending on type and duration)
- GnRH agonists/antagonists: ₹6,000–₹15,000 per injection, often given monthly
- Add-back therapy (if required): ₹800–₹2,000 monthly
These estimates can change based on brand, dosage, and follow-up needs. Mayflower offers transparent billing and helps patients select cost-effective combinations without compromising care quality.
Typical Treatment Duration
Most hormonal therapies are prescribed for 6–12 months, depending on symptom response. Some, like birth control or progestin IUDs, may be continued longer under medical supervision to prevent recurrence.
Doctors periodically review your progress through follow-up appointments and imaging if necessary. Once symptoms are well managed, therapy can be tapered or transitioned to maintenance care.
Factors Influencing Cost and Duration
- Severity and stage of endometriosis
- Type of hormone used (pill, injection, implant)
- Duration of therapy
- Additional treatments such as laparoscopy or physiotherapy
By combining medical efficiency with patient-centered transparency, Mayflower Women’s Hospital ensures that hormonal therapy remains accessible and personalized for every woman.
Now that we’ve discussed cost and duration, it’s time to explore how Mayflower’s expert gynecologists design and monitor these therapies to deliver the best outcomes.
Mayflower’s Expertise in Endometriosis Hormonal Care
Choosing the right hospital for hormonal therapy for endometriosis can make all the difference between temporary relief and lasting recovery. At Mayflower Women’s Hospital, every treatment is guided by a multidisciplinary team of gynecologists, laparoscopic surgeons, fertility experts, and nutritionists-ensuring that patients receive complete, evidence-based care.
Personalized Hormonal Therapy Plans
Each patient’s hormonal profile and medical history are unique. That’s why Mayflower’s doctors perform detailed assessments before prescribing any therapy. From selecting the right progesterone therapy for endometriosis to evaluating whether GnRH agonists are appropriate, every plan is customized to deliver maximum symptom relief with minimal side effects.
Advanced Diagnostics and Monitoring
Mayflower is equipped with advanced imaging technologies such as MRI for endometriosis and laparoscopic evaluation tools. Regular follow-ups, hormonal assays, and bone health assessments help track treatment progress and prevent long-term complications.
Integrated Care Model
Hormonal therapy is most effective when combined with holistic care. Mayflower’s specialists incorporate:
- Nutritional counseling to manage estrogen dominance
- Physiotherapy for pelvic muscle relaxation
- Mental health support for stress and pain management
- Post-treatment follow-up programs to prevent recurrence
This integrated model ensures comprehensive healing-not just symptom control.
Why Patients Trust Mayflower
- Team of the best doctors for endometriosis in India
- Decades of experience in hormonal and surgical care
- Transparent cost structure and patient-first approach
- USFDA-approved technologies for diagnosis and monitoring
Patients who undergo hormonal treatment at Mayflower often report improved quality of life, lighter menstrual cycles, and significant pain reduction within months.
To see how real patients have benefited from these therapies, let’s look at some success stories and lifestyle insights that complement hormonal care.
Patient Success Stories & Lifestyle Support
Every woman’s journey with endometriosis is unique, and so is her response to hormonal therapy for endometriosis. At Mayflower Women’s Hospital, many patients have regained comfort, balance, and confidence through individualized treatment plans.
Real-Life Patient Outcomes
One patient in her early thirties came to Mayflower after years of severe menstrual pain and failed home remedies. After a detailed evaluation, our specialists started her on progesterone therapy for endometriosis, complemented by nutritional counseling and yoga-based relaxation. Within three months, her pain intensity had reduced by nearly 70%, and her cycles became more predictable.
Another case involved a young woman with recurrent ovarian cysts who underwent GnRH agonist therapy under close supervision. Her ultrasound results showed a visible reduction in cyst size within six months, and her energy levels improved significantly after add-back therapy.
These results underline that with medical guidance, consistency, and lifestyle discipline, hormonal therapy can transform quality of life without surgery.
Lifestyle Habits That Support Hormonal Balance
Hormonal therapy works best when supported by healthy daily habits.
- Nutrition: Focus on anti-inflammatory foods like berries, salmon, flaxseeds, and leafy greens.
- Stress Management: Meditation, journaling, and deep breathing can stabilize cortisol levels that influence estrogen.
- Physical Activity: Low-impact exercises such as Pilates, cycling, or yoga help improve circulation and reduce pelvic pain.
- Sleep and Hydration: Maintaining a consistent sleep schedule and drinking enough water can further regulate hormones naturally.
Holistic Healing Approach
Mayflower integrates medical treatment with lifestyle modification programs to ensure that hormonal therapy is not just about symptom relief-but long-term recovery. Patients receive education, tracking tools, and ongoing consultations for a sustainable, empowered journey toward wellness.
Now that you’ve seen how hormonal therapy can bring real improvements, let’s summarize how this approach fits into a complete, evidence-based strategy for managing endometriosis.
Conclusion – A Personalized, Evidence-Based Approach
Hormonal therapy for endometriosis remains one of the most effective and scientifically supported ways to control pain, regulate cycles, and prevent disease progression. By targeting the hormonal imbalance that drives the condition, it allows women to regain comfort and lead active, fulfilling lives.
At Mayflower Women’s Hospital, every hormonal treatment plan is built on precision, compassion, and collaboration. Our experts combine advanced medical science with individualized attention-ensuring that each woman receives the right therapy for her unique needs and long-term health goals.
If you’ve been struggling with persistent pelvic pain, heavy periods, or fatigue, don’t ignore the signs. Early diagnosis and tailored hormonal management can make a lasting difference.
Take the first step toward relief and restoration-schedule a consultation with Mayflower’s endometriosis specialists today.
Frequently Asked Questions (FAQ)
No, hormonal therapy doesn’t cure endometriosis permanently, but it helps control the symptoms and slow down the progression of the disease. Once therapy stops, some symptoms may return. Ongoing monitoring and lifestyle management improve long-term outcomes.
Common side effects include mild weight changes, mood swings, irregular bleeding, and hot flashes. These are usually temporary and can be managed through medical supervision, diet, and lifestyle adjustments. Severe or persistent side effects should always be discussed with your doctor.
Yes, combined oral contraceptives (birth control pills) are one of the most common forms of hormonal therapy. They work by suppressing ovulation and regulating hormone levels, which helps reduce menstrual pain and endometrial growth.
Yes. Hormonal therapy is reversible and designed to suppress ovulation temporarily. Once you stop taking the medication and your natural cycle resumes, fertility typically returns within a few months. Consult your gynecologist to plan pregnancy safely after treatment.
Surgery may be recommended if hormonal therapy fails to relieve symptoms, or when cysts, adhesions, or infertility issues are present. Laparoscopic excision surgery can remove lesions effectively while preserving fertility and reducing recurrence risk.
Author
-

Dr. Smeet, true to his name, is known for his warm personality and cheerful smile that make patients instantly feel at ease with him.
Until now, he has performed 8000+ surgeries and several of which are supra-major surgeries for deep infiltrating endometriosis and fertility enhancing surgeries. With several publications in notable journals, he is constantly pushing the envelope of possibilities in gynecological surgeries