Pelvic pain causes in women range from temporary conditions like ovulation pain to more complex issues such as endometriosis, pelvic inflammatory disease, or ovarian cysts. For many, this pain is not just a physical problem but one that impacts fertility, intimacy, and quality of life.
Doctors classify pelvic pain as either acute (sudden and short-term) or chronic (lasting six months or longer). Acute pelvic pain can signal emergencies like a ruptured cyst or infection, while chronic pelvic pain often develops slowly and may persist for years. Both forms deserve medical attention.
This blog explores the seven most common causes of pelvic pain in women, explains how they present, and highlights when to seek urgent medical care. At Mayflower Hospital, our specialists stress that pelvic pain should never be ignored, as early diagnosis makes treatment more effective and prevents long-term complications.
Understanding Pelvic Pain in Women
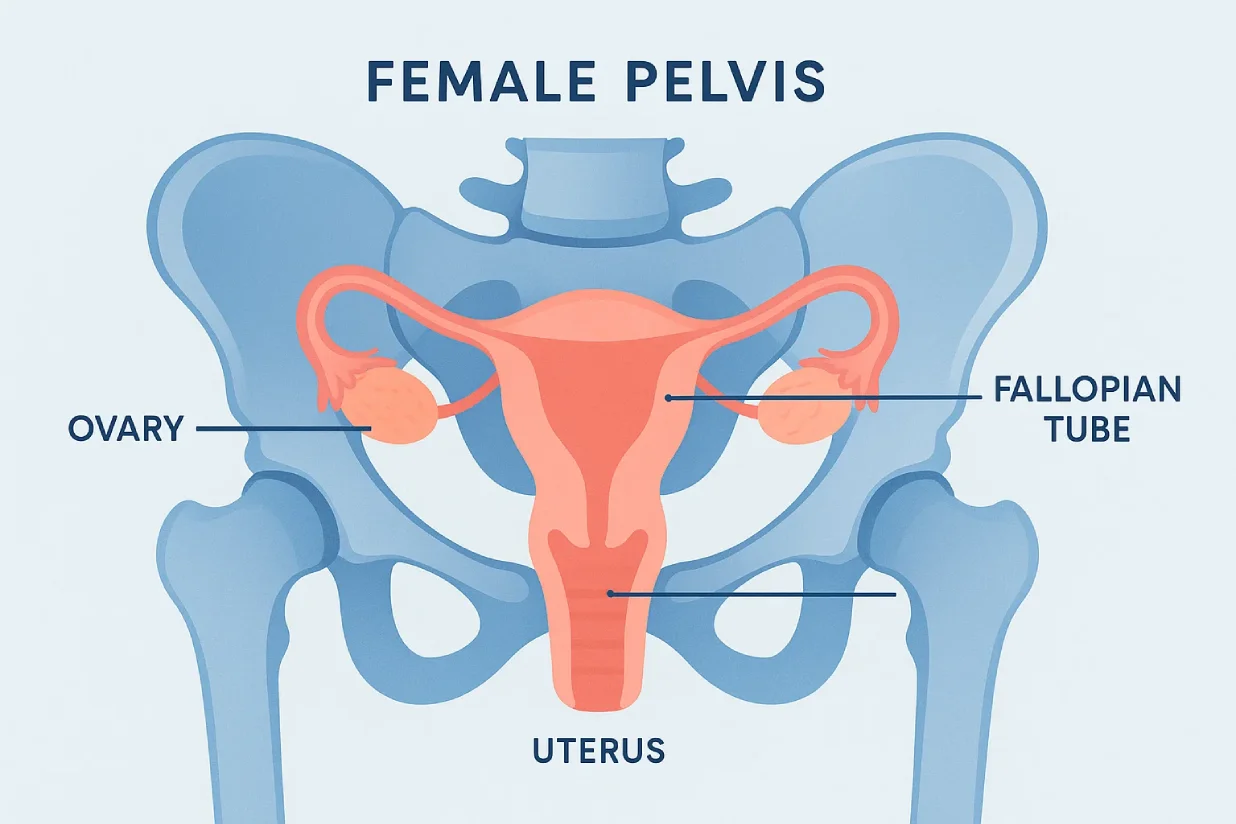
Pelvic pain in women is defined as discomfort in the lower abdomen and pelvic region, which houses the reproductive, urinary, and parts of the digestive system. Because so many organs are located in this area, pelvic pain can have multiple causes, ranging from mild to severe.
Doctors often classify pelvic pain into two main categories:
- Acute pelvic pain – Sudden in onset, lasting for hours or days, and often linked to urgent conditions like infections, ovarian torsion, or a ruptured cyst.
- Chronic pelvic pain – Persists for six months or more, recurring regularly or continuously. It is commonly associated with endometriosis, adenomyosis, or pelvic inflammatory disease.
The pain itself can vary in intensity and timing. Some women feel a dull ache during menstruation, while others experience sharp, stabbing pains that interfere with everyday life. It may occur constantly or only during specific activities such as urination, intercourse, or ovulation.
Ignoring pelvic pain can be risky. Chronic pelvic pain may affect fertility, mental health, and relationships if left untreated. Even occasional lower abdominal pain in women should be evaluated if it becomes frequent, severe, or disrupts daily routines.
At Mayflower Hospital, our gynecologists emphasize that pelvic pain should never be dismissed as “normal” or something to endure silently. Understanding its nature and recognizing patterns are the first steps toward accurate diagnosis and long-term relief.
How Pelvic Pain Feels: Types & Patterns
Pelvic pain does not always feel the same for every woman. For some, it presents as a dull ache, while for others it feels like a sudden stabbing sensation. Recognizing the types and patterns of pelvic pain provides valuable clues about its underlying causes.
Types of Pelvic Pain
- Sharp or stabbing pain – Often linked to ovarian cyst rupture, appendicitis, or other acute conditions.
- Dull, aching pain – Common with chronic pelvic pain or conditions such as adenomyosis.
- Burning or throbbing pain – May occur with infections like urinary tract infections (UTIs).
- Pressure or heaviness – Frequently reported in women with enlarged ovaries, fibroids, or pelvic organ disorders.
Patterns of Pelvic Pain
- Cyclical pain – Occurs in line with the menstrual cycle. Endometriosis symptoms and ovulation pain (Mittelschmerz) typically follow this pattern.
- Non-cyclical pain – Not tied to menstruation; can be caused by infections, scar tissue, or urinary conditions.
- Intermittent pain – Comes and goes, often triggered by physical activity, urination, or intercourse.
- Persistent pain – Continuous discomfort that may suggest chronic conditions such as endometriosis or pelvic inflammatory disease.
Because lower abdominal pain in women may mimic many different disorders, documenting how pain feels and when it occurs is important. For example, ovulation-related discomfort usually resolves within hours, while pain from endometriosis may last for days and worsen over time.
By identifying the type and pattern of pelvic pain, women can provide their doctors with crucial information that supports early and accurate diagnosis.
Lifestyle & Risk Factors for Pelvic Pain
Not every woman experiences pelvic pain for the same reasons. Certain lifestyle choices and medical risk factors can increase the likelihood of developing discomfort in the pelvic area. Understanding these influences helps in prevention and early intervention.
Hormonal Changes
Fluctuations in estrogen and progesterone affect the menstrual cycle and may trigger pelvic pain. Conditions such as adenomyosis and endometriosis symptoms often worsen during hormonal peaks, leading to severe cramps or persistent lower abdominal pain in women.
Sexual Health & Infections
Unprotected intercourse or a history of sexually transmitted infections (STIs) can increase the risk of pelvic inflammatory disease (PID), a major cause of pelvic pain and infertility. Practicing safe sex and seeking prompt treatment for infections are crucial preventive steps.
Family & Medical History
Women with a family history of endometriosis, adenomyosis, or ovarian cysts are more prone to developing these conditions. Chronic pelvic pain may also be linked to past surgeries, abdominal scarring, or pelvic adhesions.
Lifestyle Factors
- Stress – Can worsen the perception of pain and contribute to muscle tension in the pelvic floor.
- Diet & weight – High-fat, low-fiber diets may worsen hormonal imbalances, while obesity can add pressure to pelvic organs.
- Sedentary habits – Lack of physical activity weakens pelvic muscles, making pain more noticeable.
By recognizing these risk factors, women can take proactive measures such as adopting a balanced diet, maintaining safe sexual practices, and seeking medical advice early to reduce the chances of developing chronic pelvic pain.
At Mayflower Hospital, our specialists often combine medical treatment with lifestyle guidance to deliver long-term relief for patients experiencing pelvic pain.
7 Common Pelvic Pain Causes in Women
Pelvic pain in women can result from many gynecological, urinary, or gastrointestinal issues. Below are the seven most frequent pelvic pain causes, each with distinct symptoms and implications.
1. Endometriosis Symptoms
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, often on the ovaries, fallopian tubes, or pelvic walls. This tissue responds to menstrual hormones, causing inflammation, scarring, and pain.
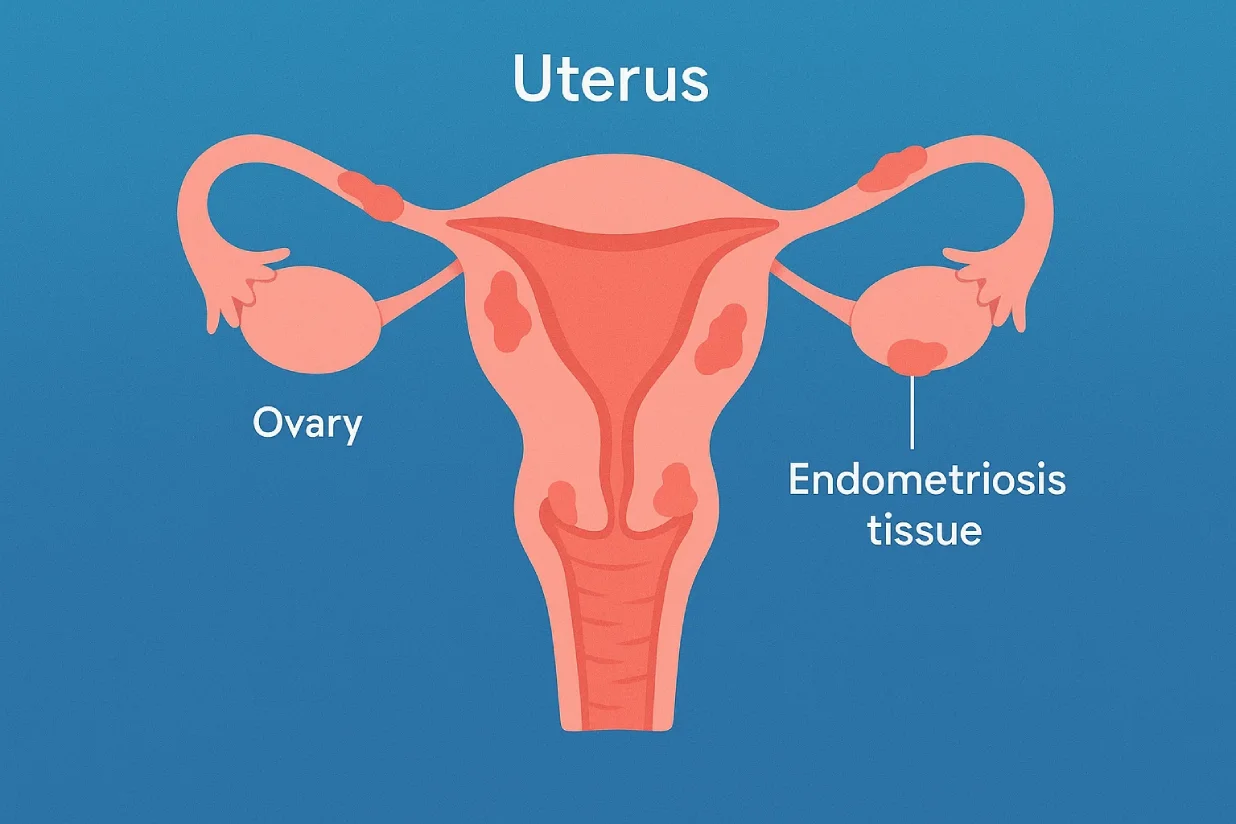
Key symptoms:
- Severe period cramps not relieved by common painkillers
- Pain during intercourse (dyspareunia)
- Difficulty conceiving
- Bowel or bladder pain during menstruation
For many women, endometriosis is a leading cause of chronic pelvic pain. Because it mimics other conditions, diagnosis often requires laparoscopy. Treatment may include hormonal medication, pain management, or minimally invasive surgery.
2. Pelvic Inflammatory Disease (PID)
PID is an infection of the female reproductive organs, usually caused by untreated sexually transmitted infections like chlamydia or gonorrhea. It damages the uterus, fallopian tubes, and ovaries, leading to long-term complications if untreated.
Key symptoms:
- Lower abdominal pain in women
- Unusual vaginal discharge with odor
- Painful urination
- Fever or chills
If left untreated, PID can cause infertility, ectopic pregnancy, and chronic pelvic pain. Early detection and antibiotics are crucial. At Mayflower Hospital, prompt treatment protocols reduce the risk of long-term damage.
3. Ovarian Cyst Pain
Ovarian cysts are fluid-filled sacs that develop on or inside the ovary. Most are harmless, but large cysts or ruptured cysts can cause significant pelvic pain.
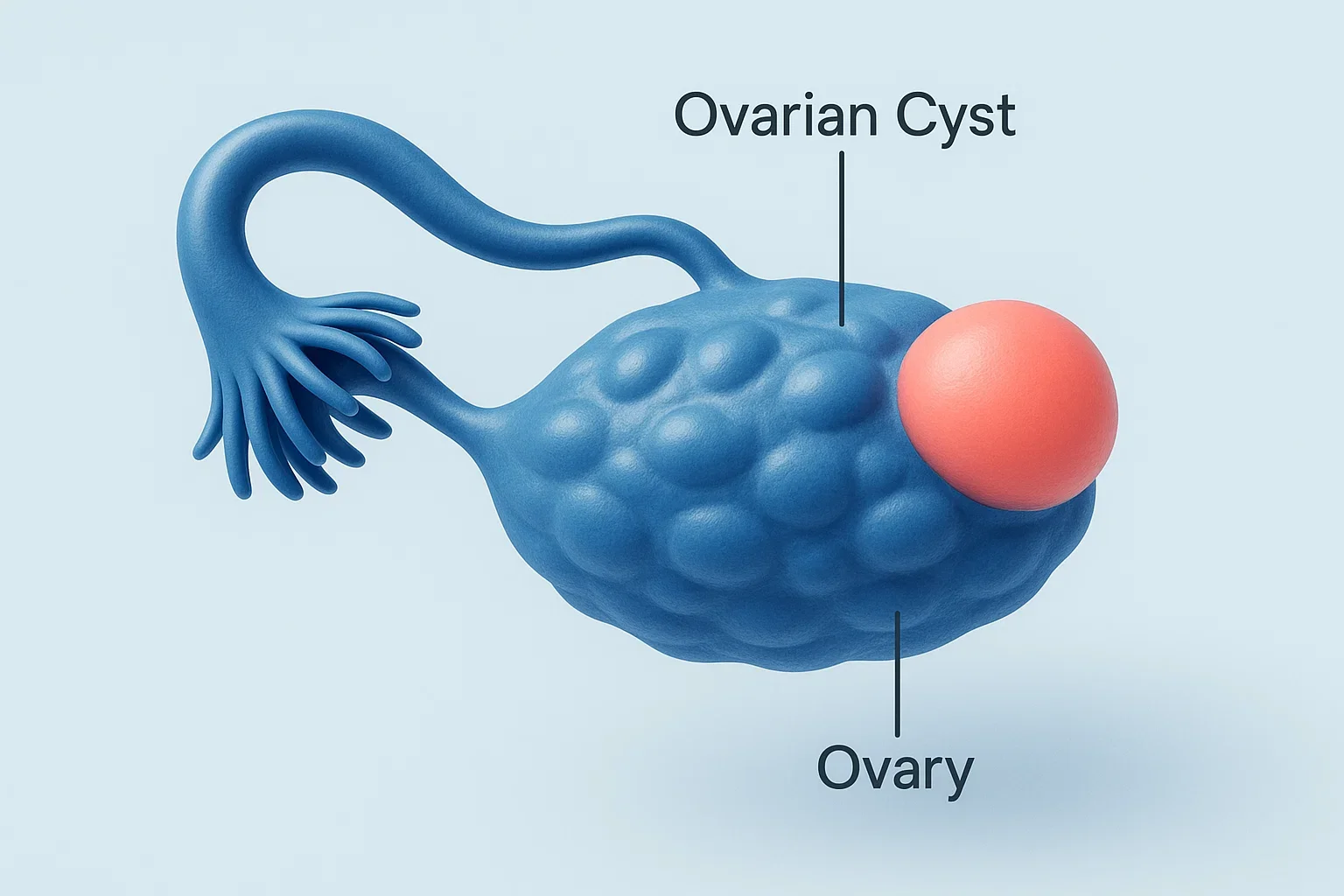
Key symptoms:
- Sudden sharp pain on one side of the pelvis
- Bloating or abdominal swelling
- Pain during intercourse
- Nausea or vomiting if rupture occurs
Small cysts often resolve naturally, but recurring or large cysts may require surgical removal. Knowing when ovarian cyst pain becomes dangerous is important especially if the pain is severe or accompanied by fever.
4. Ovulation Pain (Mittelschmerz)
Some women experience discomfort during ovulation, known as Mittelschmerz (German for “middle pain”). It happens when the ovary releases an egg mid-cycle.
Key symptoms:
- Mild to moderate pain on one side of the lower abdomen
- Occurs around day 14 of the menstrual cycle
- Lasts a few hours to a couple of days
Although usually harmless, severe or persistent ovulation pain should not be ignored. It can sometimes be mistaken for appendicitis or ovarian cysts. Keeping track of the menstrual cycle helps distinguish ovulation pain from more serious conditions.
5. Painful Sex (Dyspareunia)
Pelvic pain may also occur during or after sexual intercourse, a condition known as dyspareunia. It is often associated with underlying gynecological disorders.
Possible causes:
- Endometriosis or adenomyosis
- Vaginal dryness or hormonal changes
- Infections or pelvic floor dysfunction
Dyspareunia affects not just physical health but also emotional well-being and relationships. Identifying the underlying cause is key. Treatments may include lubricants, hormonal therapy, pelvic floor exercises, or addressing underlying medical conditions.
6. Adenomyosis
Adenomyosis happens when endometrial tissue grows into the muscular wall of the uterus, causing painful and heavy periods. It often overlaps with endometriosis, but the tissue grows inside the uterine muscle instead of outside the uterus.
Key symptoms:
- Intense menstrual cramps
- Heavy or prolonged bleeding
- Pelvic pressure or bloating
- Pain during intercourse
Unlike endometriosis, adenomyosis usually affects women in their 30s and 40s. Treatments range from pain management and hormonal therapies to hysterectomy in severe cases.
7. Urinary Tract Infections (UTIs)
Not all pelvic pain originates in the reproductive system. UTI symptoms in women often include pelvic discomfort, especially if the infection spreads to the bladder or kidneys.
Key symptoms:
- Burning sensation during urination
- Frequent urge to urinate
- Cloudy or strong-smelling urine
- Pelvic pain or pressure
Untreated UTIs can progress into kidney infections, which may cause fever, back pain, and nausea. Early diagnosis with urine tests and proper antibiotics provides quick relief and prevents complications.
Pelvic Pain vs Abdominal Pain: Key Differences
Many women confuse pelvic pain with general abdominal discomfort, but the two are not the same. Pelvic pain is located in the area below the belly button, often linked to the reproductive or urinary organs, while abdominal pain may involve the stomach, intestines, or other digestive organs. Recognizing the difference helps in narrowing down possible causes and deciding when to seek medical care.
Characteristics of Pelvic Pain
- Typically felt deep in the lower abdomen or pelvic region
- Commonly related to reproductive issues like endometriosis symptoms, ovarian cyst pain, or adenomyosis
- May worsen during menstruation, intercourse, or urination
- Can become chronic if conditions like pelvic inflammatory disease (PID) are left untreated
Characteristics of Abdominal Pain
- Can occur anywhere in the stomach or upper abdomen
- Often linked to digestive problems such as gastritis, indigestion, or gallbladder issues
- Usually influenced by food intake or gastrointestinal infections
- May improve with dietary changes or medications unrelated to gynecological care
When a woman reports lower abdominal pain, doctors first determine if it is pelvic or abdominal in origin. For example, pain after eating is more likely digestive, while pain tied to menstruation points to a pelvic cause.
Clear distinction between these two types of discomfort allows doctors to perform targeted diagnostic tests and provide the right treatment.
When Pelvic Pain Signals an Emergency

Most cases of pelvic pain in women are not life-threatening, but some symptoms should never be ignored. In certain situations, pelvic pain may indicate a medical emergency requiring immediate attention.
Warning Signs to Watch For
- Sudden, severe pain – Could signal a ruptured ovarian cyst, ectopic pregnancy, or appendicitis.
- High fever with pelvic pain – Suggests a serious infection such as pelvic inflammatory disease (PID).
- Heavy vaginal bleeding – Especially if accompanied by dizziness or fainting.
- Severe nausea and vomiting – May occur with ovarian torsion or advanced infections.
- Pain with fainting or lightheadedness – Could be linked to internal bleeding or ectopic pregnancy.
Why Urgent Care Matters
Conditions like ruptured cysts, ectopic pregnancy, or untreated PID can progress rapidly and cause complications such as infertility or even life-threatening internal bleeding. Women experiencing sudden sharp pain or worsening symptoms should not delay visiting the emergency department.
At Mayflower Hospital, our emergency and gynecology teams are trained to quickly assess, diagnose, and manage urgent cases of pelvic pain. Immediate medical care not only relieves severe discomfort but also prevents long-term complications.
Pelvic pain that escalates in intensity or appears alongside fever, fainting, or heavy bleeding should always be considered a red flag. Seeking timely medical help can save both fertility and overall health.
Diagnosis: How Doctors Find the Cause of Pelvic Pain
Because pelvic pain in women can stem from multiple conditions, accurate diagnosis is essential. Doctors rely on a combination of medical history, physical examination, and advanced investigations to determine the exact cause.
Medical History & Symptom Review
A thorough consultation helps identify pain patterns, triggers, and related symptoms. Women are asked about their menstrual cycles, history of infections, sexual activity, and family history of conditions like endometriosis or adenomyosis. Keeping a pain diary is often recommended to track whether discomfort is cyclical or persistent.
Blood & Urine Tests
Laboratory tests play a vital role in detecting infections, hormonal imbalances, and urinary tract problems. For example, urine analysis can confirm UTI symptoms in women, while blood tests may point toward inflammatory markers associated with pelvic inflammatory disease (PID).
Imaging (Ultrasound, MRI)
Ultrasound is often the first-line imaging tool to detect ovarian cyst pain, fibroids, or adenomyosis. For complex conditions like endometriosis symptoms, an MRI scan may be recommended, as it provides a clearer view of pelvic structures and deep tissue growth.
Laparoscopy
In cases where imaging is inconclusive, doctors may recommend laparoscopy. This minimally invasive procedure uses a small camera inserted through the abdomen to directly visualize reproductive organs. It is the gold standard for diagnosing endometriosis and assessing the extent of pelvic damage.
Comprehensive Evaluation at Mayflower
At Mayflower Hospital, diagnosis is never one-dimensional. Specialists use a multidisciplinary approach, combining gynecology, radiology, and laboratory expertise to deliver accurate results. This ensures women receive the right treatment plan without unnecessary delays.
Treatment Options for Pelvic Pain in Women
Treatment for pelvic pain in women depends on its underlying cause. While some conditions respond well to medication, others may require surgical intervention. Doctors at Mayflower Hospital use tailored treatment plans that focus on both symptom relief and long-term health.
Medications and Non-Surgical Approaches
- Pain relievers – Over-the-counter NSAIDs (non-steroidal anti-inflammatory drugs) are often used to manage period-related pain or mild ovarian cyst pain.
- Antibiotics – Prescribed when pelvic pain is due to infections such as pelvic inflammatory disease (PID) or urinary tract infections.
- Hormonal therapy – Birth control pills, IUDs, or hormone injections help regulate cycles and reduce symptoms linked to endometriosis symptoms and adenomyosis.
- Physical therapy – Pelvic floor exercises and relaxation techniques relieve pain related to muscle tension.
Surgical Options
- Laparoscopy – Used to diagnose and treat endometriosis, remove ovarian cysts, or release scar tissue.
- Hysteroscopy – Helps treat uterine problems, including polyps or fibroids that contribute to pelvic pain.
- Hysterectomy – In severe cases of adenomyosis or chronic pelvic pain unresponsive to other treatments, removal of the uterus may be considered.
- Cyst removal surgery – Recommended if large ovarian cysts cause persistent discomfort or complications.
Multidisciplinary Care
For women with chronic pelvic pain, a single treatment may not be enough. A combination of medication, surgery, counseling, and physiotherapy often provides the best results. At Mayflower Hospital, specialists work collaboratively to ensure every woman receives personalized care suited to her condition and lifestyle needs.
Managing pelvic pain effectively requires both short-term relief and long-term strategies. With the right treatment, most women can regain comfort, improve fertility outcomes, and enhance overall quality of life.
Lifestyle, Home Remedies & Prevention
Along with medical treatment, certain lifestyle adjustments and home remedies can reduce pelvic discomfort and prevent flare-ups. While these approaches may not cure underlying conditions like endometriosis or adenomyosis, they support overall pelvic health and improve daily comfort.
Home Remedies for Relief
- Heat therapy – Applying a warm compress or heating pad to the lower abdomen helps relax muscles and ease menstrual cramps.
- Gentle exercise – Activities like yoga and walking improve blood flow and reduce stiffness linked to chronic pelvic pain.
- Hydration – Drinking enough water supports urinary tract health and lowers the risk of recurrent UTI symptoms in women.
- Stress reduction – Meditation, deep breathing, and relaxation techniques can decrease muscle tension and pain perception.
Preventive Lifestyle Measures
- Balanced diet – Consuming anti-inflammatory foods such as fruits, vegetables, and whole grains may help regulate hormones and reduce painful episodes.
- Safe sexual practices – Using protection lowers the risk of infections that may lead to pelvic inflammatory disease (PID).
- Regular health check-ups – Early screenings and routine gynecological visits ensure prompt detection of problems like ovarian cysts or infections.
- Weight management – Maintaining a healthy body weight decreases excess pressure on the pelvic organs.
By combining medical care with preventive steps, women can reduce the frequency and intensity of pelvic pain while improving long-term reproductive health.
Living with Pelvic Pain – Coping Strategies
For women living with chronic pelvic pain, treatment is often a journey rather than a quick fix. Beyond medical and surgical care, adopting practical coping strategies can help manage discomfort and improve emotional well-being.

Emotional Support and Counseling
Chronic pelvic pain is not only physical but also emotional. Anxiety, depression, and relationship challenges are common. Counseling or support groups can provide women with coping skills and reassurance that they are not alone.
Physiotherapy and Body Awareness
Pelvic floor physiotherapy teaches women how to relax tense muscles, strengthen weak areas, and reduce pain during activities such as intercourse or exercise. Learning body mechanics can also minimize strain on the lower abdomen.
Daily Self-Care Habits
- Scheduled rest – Balancing activity and downtime prevents pain flare-ups.
- Mind-body techniques – Meditation, mindfulness, and breathing exercises reduce stress-related muscle tension.
- Routine journaling – Tracking symptoms helps women and doctors identify patterns, making treatment more effective.
Integrative Approaches
Complementary practices such as acupuncture, massage, or relaxation therapies may provide additional relief when combined with medical treatment.
At Mayflower Hospital, care plans for women with chronic pelvic pain include not just medication or surgery but also guidance on lifestyle and coping strategies, ensuring a holistic approach to healing.
Personalized Care for Women with Pelvic Pain at Mayflower
Every woman’s experience of pelvic pain is unique, which is why a personalized approach to diagnosis and treatment is essential. At Mayflower Hospital, our team of gynecologists, radiologists, and surgeons work together to provide comprehensive care tailored to each patient’s needs.
Advanced Diagnostic Tools
We use modern imaging techniques such as ultrasound and MRI, along with minimally invasive procedures like laparoscopy, to accurately identify conditions such as endometriosis, adenomyosis, or ovarian cyst pain.
Individualized Treatment Plans
Treatment may involve medication, physiotherapy, or advanced surgical options, depending on the diagnosis. For women with chronic pelvic pain, our care goes beyond medical intervention, including counseling, lifestyle advice, and rehabilitation support.
Compassionate Women-Centered Care
We understand that pelvic pain affects not only the body but also emotions, relationships, and daily routines. Our specialists emphasize compassionate care, ensuring women feel supported throughout their journey toward recovery.
At Mayflower Hospital, the focus is always on helping women regain comfort, improve reproductive health, and enhance quality of life through evidence-based, individualized treatment.
Why Choose Mayflower Hospital for Pelvic Pain Treatment?
Choosing the right hospital for managing pelvic pain in women makes a significant difference in outcomes. At Mayflower Hospital, we combine medical expertise with advanced technology to ensure women receive accurate diagnosis and effective treatment.
Expertise in Women’s Health
Our gynecology team has years of experience in treating complex conditions such as endometriosis symptoms, pelvic inflammatory disease (PID), adenomyosis, and ovarian cyst pain. This specialization allows us to handle both routine and high-risk cases with precision.
Advanced Facilities
We offer minimally invasive procedures, including laparoscopy and hysteroscopy, which reduce recovery times and minimize discomfort. State-of-the-art imaging tools like ultrasound and MRI ensure accurate detection of underlying causes of chronic pelvic pain.
Patient-Centered Approach
At Mayflower, treatment is never one-size-fits-all. Each woman receives a tailored plan designed to address her specific health concerns, lifestyle, and future fertility goals.
By combining compassionate care with medical excellence, Mayflower Hospital has become a trusted choice for women seeking lasting relief from pelvic pain.
If you are experiencing persistent pelvic pain, schedule a consultation with our specialists today to find the right treatment and regain control of your health.
Conclusion
Pelvic pain causes in women can vary from temporary conditions like ovulation pain (Mittelschmerz) to complex disorders such as endometriosis, adenomyosis, or pelvic inflammatory disease (PID). While some discomfort may resolve on its own, chronic or severe pain should never be ignored. Early diagnosis allows for effective treatment, prevents complications, and helps protect fertility and overall health.
At Mayflower Hospital, we are committed to providing accurate diagnosis, personalized treatment, and compassionate care for every woman experiencing pelvic pain. If you or a loved one are struggling with persistent symptoms, consult our specialists today to find relief and restore your quality of life.
Frequently Asked Questions (FAQs)
The most frequent causes include endometriosis symptoms, pelvic inflammatory disease (PID), ovarian cyst pain, adenomyosis, ovulation pain (Mittelschmerz), and urinary tract infections (UTIs). Each has distinct symptoms, but all require medical evaluation if pain is persistent.
Yes. Endometriosis is one of the leading causes of chronic pelvic pain. The misplaced tissue bleeds and scars with every menstrual cycle, leading to inflammation and long-term discomfort.
Seek medical care if pelvic pain is sudden, severe, or associated with fever, nausea, heavy bleeding, or fainting. These symptoms may indicate emergencies such as a ruptured cyst, ectopic pregnancy, or untreated PID.
Doctors use a combination of blood tests, urine analysis, ultrasound, MRI, and laparoscopy to identify causes. The choice of tests depends on symptoms and medical history.
Yes. Heat therapy, gentle exercise, hydration, and stress management can ease mild pelvic pain. However, these should complement not replace medical treatment, especially when conditions like endometriosis or adenomyosis are involved.
Author
-

Dr. Smeet, true to his name, is known for his warm personality and cheerful smile that make patients instantly feel at ease with him.
Until now, he has performed 8000+ surgeries and several of which are supra-major surgeries for deep infiltrating endometriosis and fertility enhancing surgeries. With several publications in notable journals, he is constantly pushing the envelope of possibilities in gynecological surgeries